Broadening Horizons for Bispecific Effector Cell Redirection
2022 has been a successful year for bispecifics, with the FDA’s approval of Faricimab and Tebentafusp to make up a total of five bispecific molecules to reach the market so far. But when it comes to effector cell redirection, there remain only two approved molecules. The effector cell redirection field appears be standing in the shadows of the CAR T field, which so far boasts a total of six approvals.
Valued at 1,965.8 million USD in 2021, the global CAR-T therapy market is expected to reach 3,150 million USD in 2025, at a CAGR of 24.9%. Whilst it may look like the CAR T market is dominating the wider biologics field, effector cell engagers and redirection remain a vital engine in cancer immunotherapy.
And it was during Oxford Global’s annual Biologics UK: In-Person event in March 2022 that key industry opinion leaders from some of the most well-renowned pharmaceutical companies gathered to discuss the priorities, challenges, and future opportunities of effector cell redirection and cell engagers. This article covers some of the critical discussions covered, with exclusive insights from Stefan Zielonka, Director of Protein Engineering & Antibody Technologies at Merck Healthcare KGaA and Suzanne Bal, Scientist at Merus.
Distinguishing Cell Engager Activity:
“Given the differences in the number of approved CAR therapies vs bispecifics for effector cell direction one could ask: Is there still room for bispecific effector cell engagers?” Zielonka stated. “And if you have the opportunity to do both, when do you decide which path to take?” There is no one-size-fits-all when it comes to selecting the correct type of cell engagement for the appropriate clinical purpose; each has its own set of unique attributes and disadvantages.
- Harnessing Bispecific T Cell Engagers and T Cell Primers in Cancer Treatment
- Addressing the Future of Bispecific and Multi-Specific Antibodies
- Discover Alligator Bioscience AB and Apteov Therapeutics Inc’s Joint Bispecific Antibody
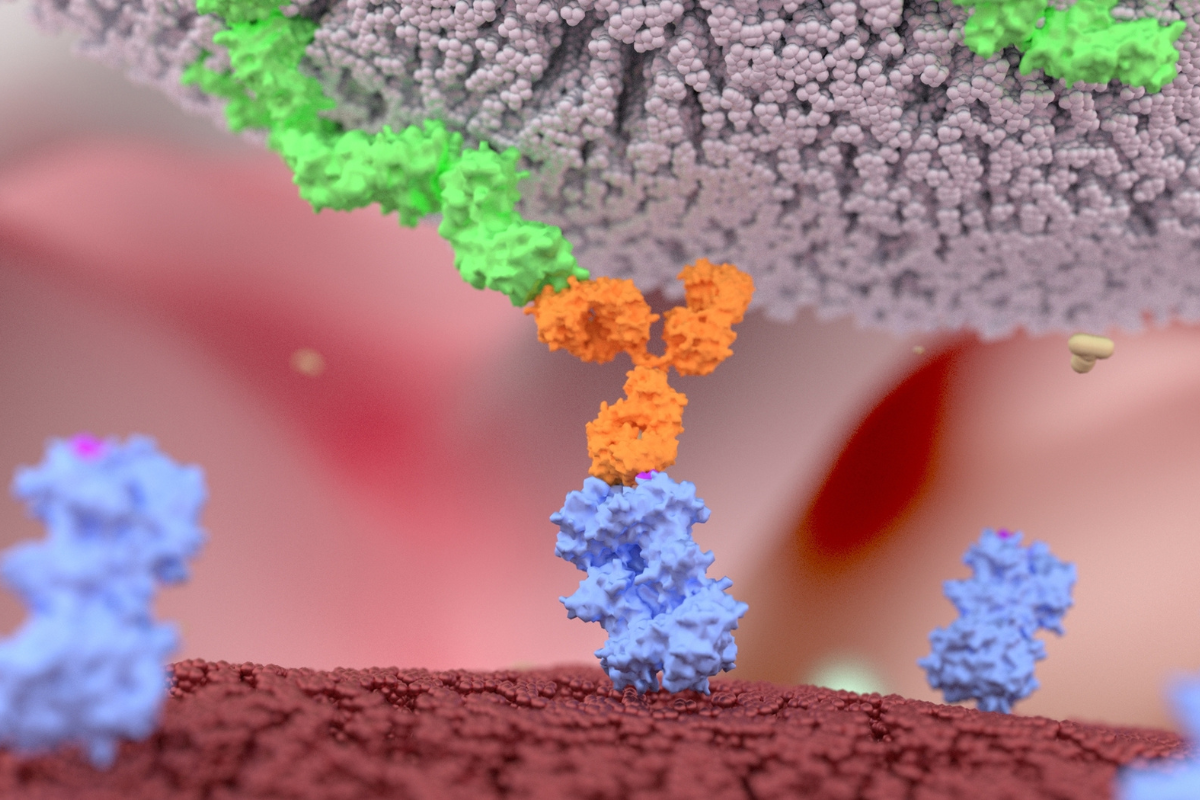
As Bal puts it, “bipecifics are most promising for haematological indications”. The proximity of a tumour-specific antigen and an effector cell antigen produces a targeted activation of effector cells. In fact, most clinical pipelines for haematological indications are mainly bispecific.
Bispecifics T cell-engagers prove a valuable tool in solid tumour targeting. They work to ensure the efficacy of cancer treatment efficacy engaging and mobilising T cells to eradicate malignant cells. Bispecifics T cell-engagers hamper tumour immune escape and block immunosuppressive molecules, including programmed cell death 1 (PD-1) and its ligand (PD-L1). By releasing cytotoxic T cells to eliminate tumour cells, such engagement can transform clinical practice for oncology.
Getting Cytokine Release Under Control:
Recent progress in getting custom domains into the clinic and advances in cytokine support is set to put bispecifics on an equal playing field with CAR Ts. While moderate cytokine production can be advantageous with respect to targeted inflammation of tumours, excessive release is a common drawback associated with T cell-therapies and therapeutic antibodies, resulting in adverse events such as organ dysfunction.
“Given the differences in the number of approved CAR therapies vs bispecifics for effector cell direction one could ask: Is there still room for bispecific effector cell engagers?”
“You want to get your molecules as active as possible to trigger the T cells,” Zielonka explains. “However, this comes with the drawbacks of toxicities such as cytokine release syndrome for T cell engagers,” he added. To combat this effect, stearic acid glucose such as Dexamethasone can be introduced in the clinic, as well as anti-IL6 agent antibodies. Other opportunities include following up T cell activation with a cytokine-related checkpoint inhibitor to minimise receiving these negative signals.
Creating safer molecules provides a further opportunity to curb harmful cytokine release. This would involve discovering cytokine release-associated in vitro assays to implement within the initial stages of drug development. According to Zielonka, “it's about finding that sweet spot to determine how much cytokine release is needed for a given indication.” Bal concurred, stating that “early identification of a molecule with low cytokine production and good licensing possibilities may lead to optimal results.”
Nevertheless, critical considerations for this approach include protentional issues with translation. For instance, as Bal explains, “it will be necessary to establish best practices for testing the assay for cytokine release in a physiologically relevant manner.” This is because assay development in a petri dish and mouse model cannot sufficiently activate cell infiltration. Patient heterogeneity may also present a bottleneck in this area.
Effective Cell Redirection Beyond Conventional Alpha Beta T-Cells:
The horizon for cell redirection in bispecifics continues to expand. In moving away from conditional and conventional T cell engagers, the field has achieved accelerated success with NK Cell engagers in particular. For instance, the biotechnology company Innate Pharma are presently collaborating with AstraZenenca to bring Monalizumab into the clinic (actually this molecule is in phase III, so to approval might be better wording). Monalizumab is a potentially first-in-class immune checkpoint inhibitor targeting NKG2A receptors expressed on tumour infiltrating cytotoxic CD8+ T cells and NK cells.
Adopting a more expansive and comprehensive approach is set to become the new normal for bispecific engagement and redirection.
Lava Therapeutics are using Gamma Delta T cell engagers for haematological disease treatments. LAVA-051, in its unique activation of both V?9V?2 (Vgamma9 Vdelta2) T cells and invariant natural killer T (iNKT) cells, is in phase I clinical trials. Broader approaches include CD40 for effector cell redirection, which is a protein-coding gene belonging to the Tumour Necrosis Factor-receptor (TNF) family found on antigen-presenting cells of the immune system.
Future Perspectives in Bispecific T Cell Redirection:
Adopting a more expansive and comprehensive approach is set to become the new normal for bispecific engagement and redirection. It can be crucial to use different cells to fully complement different antibodies’ functions. Benefits include pathogenic priming and the ability to harness tumour remodelling. Other exciting areas of development in the field include targeting suppressive cells in the tumour microenvironment.
As we move into the future of cell redirection and engagement, producing off-the-shelf bispecifics with a proven safety profile will become a top priority to ensure greater accessibility. Considerable efforts are also being made in using combined molecules to achieve a controlled cytokine release rate to achieve maximum therapeutic efficacy. If Biologics UK: In-Person has taught us anything, it's that the cell redirection and engager market is one of burgeoning promise.
Join Oxford Global's next Biologics UK: In-Person event today. This 3-day conference brings together a panel of prominent leaders and scientists, sharing new case studies, innovative data and industry outlook.