Spatial Analysis of TME Microglia in Melanoma Brain Metastasis
Presented by: Dave Hoon, Director of Translational Research at Saint John’s Cancer Institute
Edited by: Ben Norris
Until recently, melanoma brain metastases (MBMs) were viewed as being untreatable, with available therapies offering palliative care at best. Historic challenges in treating brain metastases have included the difficulties associated with penetrating the blood-brain barrier for systemic therapies. Now, immunotherapies have been identified as a potential means of treatment, with initial trials appearing to show better penetration into the central nervous system (CNS).
- Now Available: Oxford Global's R&D Key 40 Stories
- Confronting Antibody-Mediated Rejection Through Precision Medicine
- Data Collection and Spatial Analysis: Quality Control for Quality Data
Dave Hoon, Director of Translational Research at St John's Cancer Research, explained to the audience at Boston's NextGen Omics US: In-Person event that the brain’s immune response could have the solution. A study carried out by his research team found that the therapeutic targeting of tumour microenvironment (TME) microglia activity may improve immunotherapy effectiveness.
Addressing Melanoma Brain Metastasis
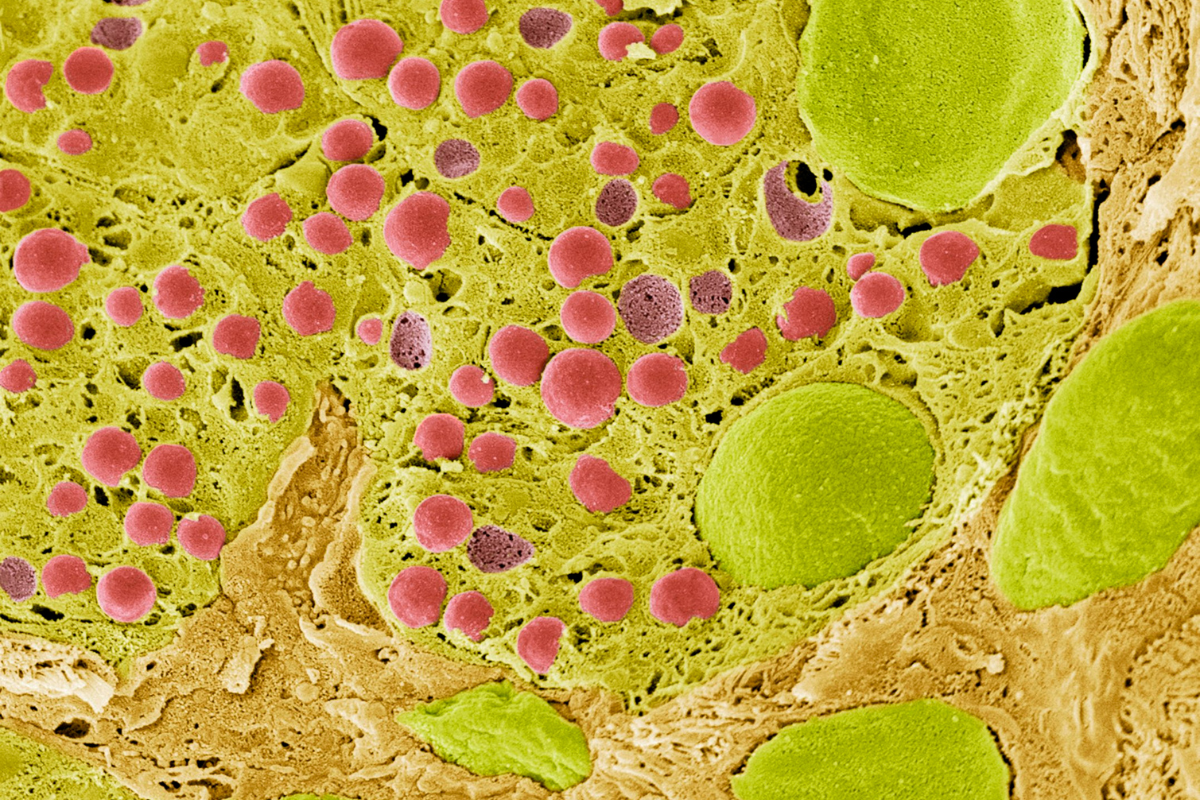
The study of the functionality and operation of microglia could be crucial to developing an effective immunological response to metastatic melanomas. “Microglia are an important part of the brain,” said Hoon. “Basically, they are its resident immune cells.” As such, microglia are important cell types in coordinating neuroinflammation, brain function, and organisation.
Microglia also play a significant role in the brain as they exhibit many immune functions, including the activation of various pathways. They are responsible for controlling and sublimating metastatic tumours. However, recent studies suggest that microglia cells induce phenotypic changes in melanoma cells which increase their malignant phenotype.
“Microglia are an important part of the brain – they are basically its resident immune cells.”
Hoon explained that melanomas had various stages in their progression to metastasis. Following its initiation in the tissue basement membrane between the epidermis and the dermis, a melanoma spreads through radial growth into the dermal layer. “The most critical stage is metastatic melanoma, where you have very aggressive disease,” said Hoon. “It can be very difficult to combat.”
Hoon explained that key diagnostic factors of MBMs include the size of the tumoral metastasis, the number of individual metastases, and the anatomical sites of tumours in the brain. “To this day, there is no effective drug treatment,” he added. “Surgery offers palliative alleviation of the disease, but there is still an issue overall.”
Immune Checkpoint Inhibitors and Study Aims
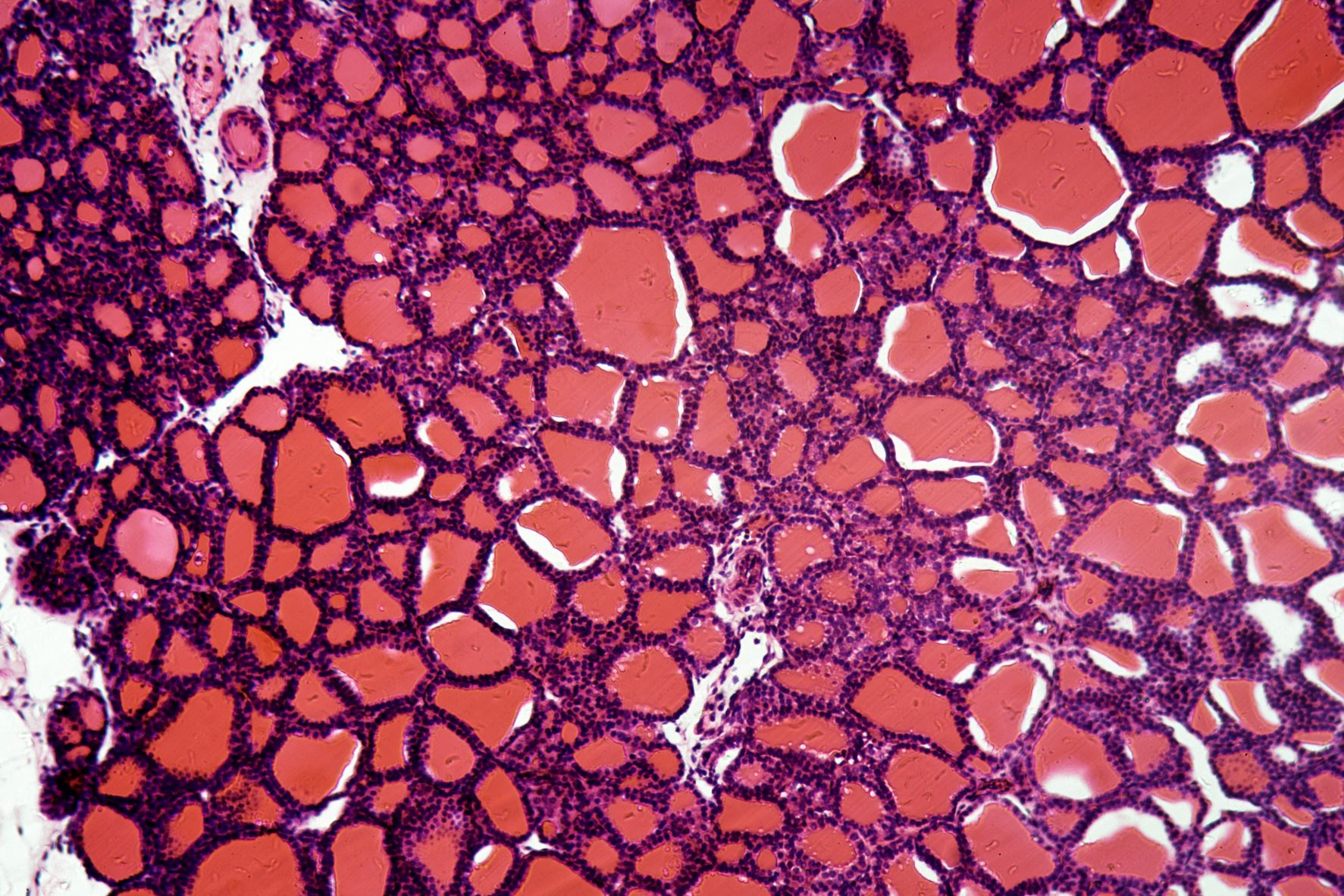
Melanoma brain metastasis is typically associated with a poor prognosis in patients. One means of combating the growth and progression of MBMs may be immune checkpoint inhibitors (ICIs). Hoon mentioned a study carried out with NanoString technology and segmentation within regions of interest (ROIs) through morphological markers. “Usually you can do about 12 ROIs per section, and usually sections are quite small,” he elaborated. “Particularly with brain melanomas.” ICIs have been approved by regulatory bodies such as the FDA for use in treating cutaneous metastatic melanoma patients to coordinate an immune response.
“ICIs are well known to halt the progression of disease,” continued Hoon. “There are few cases of a cure, but they do make for a significant prolonging of survival.” Having established the functionality of ICIs, Hoon then moved on to a comparison of patients who received ICI treatment and patients who did not receive ICI treatment but instead received surgery. He told the audience that ROI transcriptomic analysis of MBM cells and TME microglial cells revealed some clustering, divided across two different types with two different markers.
Non-ICI-treated MBM exhibited larger expressions across tissue sections compared to ICI-treated MBM, so at a fundamental level it appeared to have been treated. One of the main observations was that the gamma interferon – a cytokine critical to both innate and adaptive immunity – was down in ICI-treated TME microglia.
Future Implications for the Spatial Analysis and Treatment of Melanomas
Before rounding off his presentation, Hoon discussed the cytokine signalling pathway analysis of microglial cells. Known chemokine pathway gene activities that played roles in cancer progression were not found to be differentially expressed between ICI-treated and non-treated MBM patients.
Data on the interactions between metastatic melanoma cells and the roles of microglia-mediated neuroinflammation in facilitating melanoma brain metastasis are still limited at present. Existing observations and findings suggest that melanoma cells exert significant morphological changes on microglia cells, including enhanced proliferation and cell migration.
Hoon concluded that therapeutic targeting of TME microglia activity may improve the efficacy of immunotherapeutic treatments for melanoma brain metastasis. “In the future, microglia may be an important target to focus on, rather than just something to be removed to control brain metastasis.”
Visit our Omics Portal to learn more about the latest research into metastatic tumour treatment and new approaches to cancer treatments. If you’d like to register your interest in our upcoming Spatial Biology UK: In-Person event, click here.