Oncolytic Virus Immunotherapy: A Revolutionary Approach in Immuno-Oncology

The field of immuno-oncology is constantly evolving, with scientists tirelessly working towards groundbreaking discoveries. One such promising area is oncolytic virus immunotherapy. Defined as the use of viruses that selectively target and kill cancer cells without harming normal cells, oncolytic virus immunotherapy harnesses the natural properties of certain viruses to combat malignancies. Its purpose in immuno-oncology is twofold: to directly destroy cancer cells and to stimulate the body's immune system to launch a robust response against the tumor. For those deeply invested in immunotherapy, this is an arena filled with potential.
How does oncolytic virus immunotherapy work?
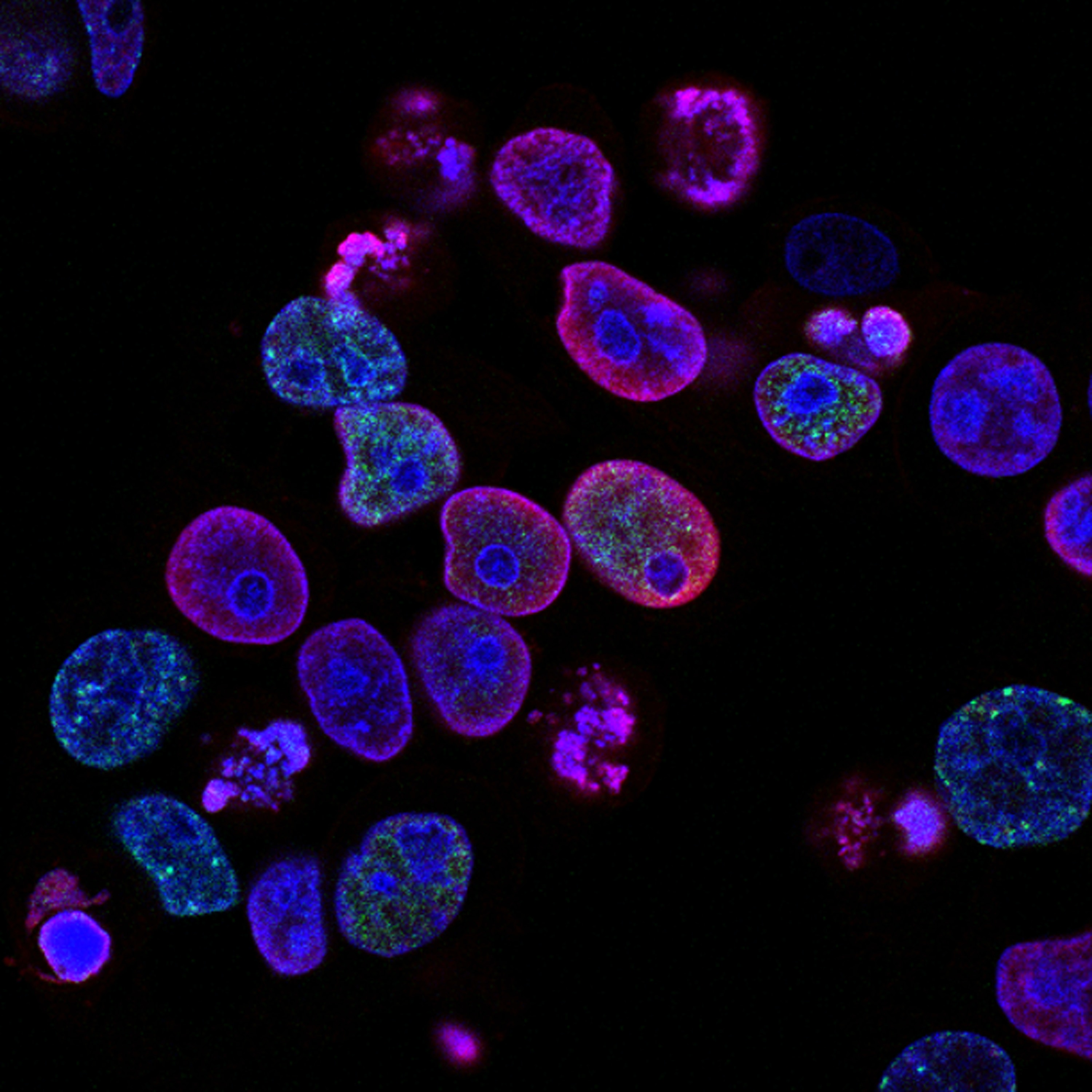
Oncolytic viruses are a specialized class of viruses that have been either naturally selected or genetically engineered to target cancer cells selectively without harming normal cells. Their mechanism of action involves multiple steps. Initially, the viruses bind to specific receptors present predominantly on cancer cells. After binding, they enter the cells and begin to replicate. This replication within the confines of the cancer cell results in an increased internal pressure, leading to the eventual bursting or lysis of the tumor cell. The release of tumor-specific antigens, coupled with viral particles, stimulates a potent immune response. This response not only targets the infected cancer cells but also other tumor cells in the body.
The therapeutic potential of oncolytic viruses goes beyond mere cell destruction. The process of cancer cell lysis releases not only the progeny viruses to infect neighboring tumor cells but also a plethora of tumor-specific antigens. These antigens are then recognized by the patient's immune system. Along with the inflammatory signals from viral infection, they mount a potent antitumor immune response. An exemplar of this is the oncolytic herpes simplex virus (T-VEC) which, besides killing melanoma cells, has also shown to boost the action of immune checkpoint inhibitors, amplifying the body's own defense against the tumor.
What are the side effects of oncolytic virus cancer vaccines?
While oncolytic virus therapies are heralded for their target specificity, they are not entirely without side effects. The body recognizes the viruses as foreign invaders, leading to an immune response that manifests as flu-like symptoms. These can include fever, fatigue, chills, and muscle aches. In essence, these symptoms can be viewed as evidence that the therapy is activating the immune system.
However, not all reactions are benign indicators of activity. There's a risk of the virus infecting non-targeted cells, leading to secondary infections. Additionally, as the immune system gears up to fight the virus, it can sometimes lead to excessive inflammation, causing complications such as organ damage or an exacerbated autoimmune response. Another noteworthy point is the interaction of oncolytic viruses with pre-existing medications or therapies. For instance, patients on antiviral medications might find reduced efficacy of the oncolytic virus treatment.
While these side effects might sound concerning, it's essential to contrast them with the often more severe and systemic side effects of traditional chemotherapy or radiation. Furthermore, ongoing research aims to refine the selectivity and safety profile of these viruses, making them even more precise in their targeting in the future.
Which cancers can be treated with oncolytic virus immunotherapy?
Oncolytic viruses represent a groundbreaking approach for cancer therapy and have demonstrated efficacy against a variety of cancers. Notably, melanoma has been a primary target, with T-VEC (Talimogene laherparepvec), an oncolytic herpes virus, becoming the first FDA-approved oncolytic virus therapy for advanced melanoma. Moreover, clinical trials have investigated oncolytic viruses against head and neck cancers, with adenoviruses and reoviruses among the prominent viral agents being explored.
Certain brain tumors, like glioblastoma, have also been targets for oncolytic virus immunotherapy. For instance, the PVSRIPO virus, a modified form of the polio virus, has undergone trials for glioblastoma and showcased an ability to improve patient survival rates.
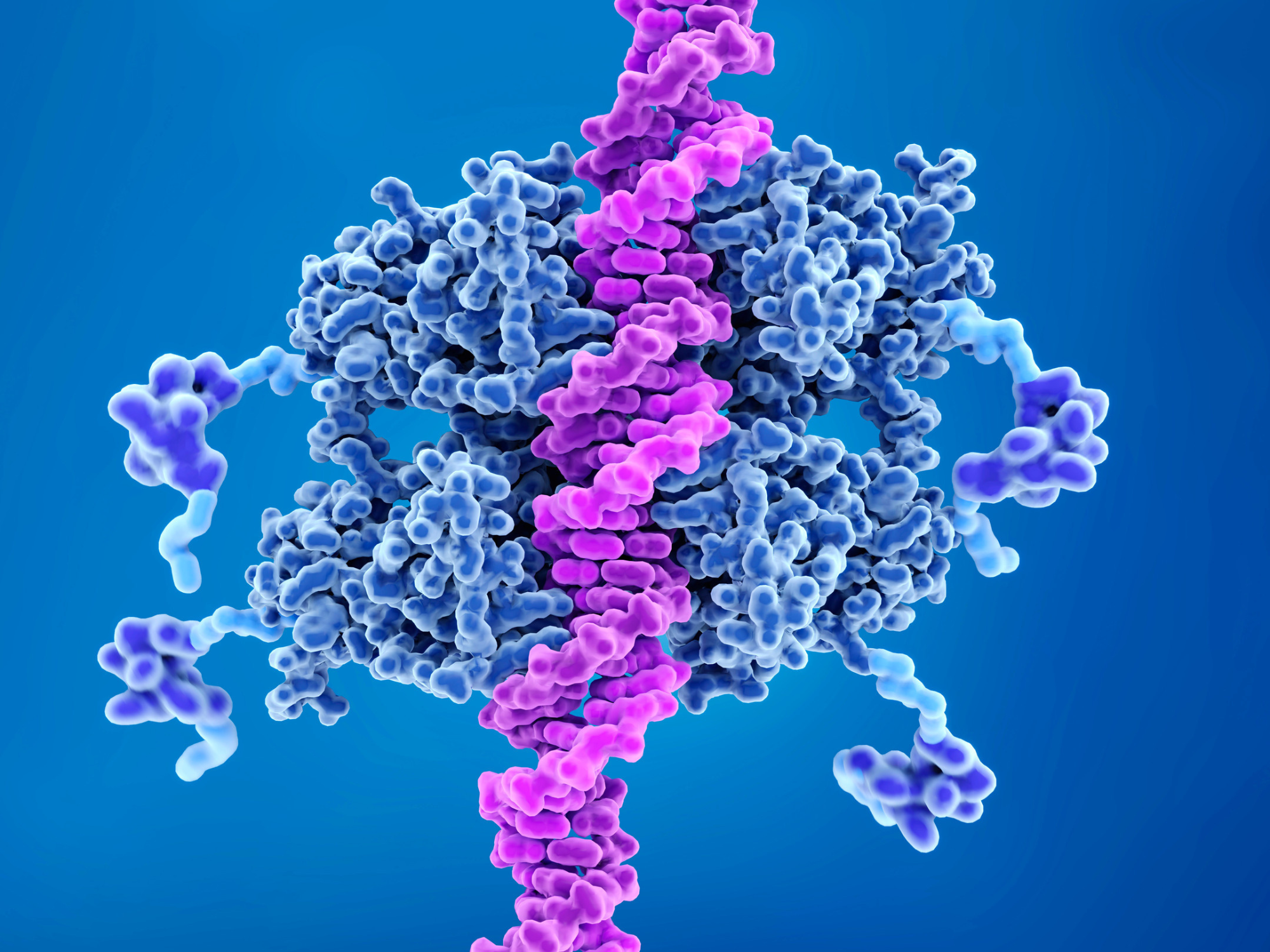
The adaptability of viruses allows scientists to genetically modify them, tailoring their properties to target specific cancer cell vulnerabilities. This vast potential means that as we understand more about the molecular intricacies of different cancers, the repertoire of oncolytic viruses and their applicability to various malignancies will only grow.
What is the success rate of oncolytic virus cancer vaccines?
The efficacy of oncolytic virus therapies isn't a one-size-fits-all answer. Different malignancies, stages of disease progression, and the genetic makeup of the tumor all play crucial roles in determining treatment outcomes. For instance, the aforementioned T-VEC has showcased response rates of about 26% in patients with advanced melanoma in certain studies.
Furthermore, the real promise of oncolytic viruses often shines when combined with other therapeutic modalities. The integration of oncolytic viruses with immune checkpoint inhibitors, drugs that unmask cancer cells to the immune system, has shown synergistic effects. For instance, a combination of oncolytic viruses with PD-1 inhibitors has been shown to enhance response rates in melanoma patients.
However, it's vital to understand that while initial and early-stage clinical trials offer hope, the success rate across a broader population can vary. Factors such as the tumor's microenvironment, the patient's overall health, and any pre-existing immunity to the virus can influence therapeutic outcomes. In sum, while oncolytic virus immunotherapy represents a transformative approach in cancer care, its efficacy is multifaceted, relying on the confluence of patient, tumor, and treatment specifics.
Are there clinical trials for oncolytic virus immunotherapy?
The landscape of oncolytic virus immunotherapy is dotted with numerous clinical trials at various stages, each seeking to understand, refine, and amplify the efficacy of these novel agents against diverse malignancies. Spanning across phases I to III, these trials encompass both standalone treatments and combination regimens.
Leading biotech and pharmaceutical companies, recognizing the potential of oncolytic viruses, have invested significant resources in their research and development. For instance, as mentioned previously Amgen's T-VEC (Talimogene laherparepvec) is one of the trailblazers, having already received FDA approval for advanced melanoma after successful clinical trials. However, T-VEC is just the tip of the iceberg. Many other oncolytic viruses, like the reovirus (Reolysin), coxsackievirus, and vesicular stomatitis virus, are in various trial stages for multiple cancers.
Additionally, some trials are exploring how oncolytic viruses can be synergistically combined with other treatments. A promising area is the confluence of oncolytic viruses with immune checkpoint inhibitors, aiming to enhance the immune system's capability to detect and destroy cancer cells. For researchers, clinicians, and patients keen on tracking the progress of these trials or exploring opportunities for participation, platforms like ClinicalTrials.gov serve as comprehensive repositories. The site, managed by the U.S. National Library of Medicine, provides detailed information on each trial's objective, methodology, stage, and current status. It's an essential tool for anyone looking to stay abreast of the latest developments in oncolytic virus immunotherapy.
Conclusion
The transformative potential of oncolytic virus immunotherapy cannot be understated in the ever-evolving realm of immuno-oncology. Leveraging the innate and adaptive immune system against cancer has always been a coveted goal, and oncolytic viruses are turning this aspiration into reality. By causing direct tumor cell lysis and sparking a cascade of immune responses, they offer a dual-pronged attack against malignancies.
Historical landmarks, like the FDA approval of T-VEC for melanoma, serve as testament to the strides made in this field. Moreover, ongoing research, as evidenced by the plethora of clinical trials, is honing these agents for increased specificity, potency, and safety. Collaborative efforts, like the combination of oncolytic viruses with immune checkpoint inhibitors or CAR-T cell therapies, are setting the stage for multimodal approaches that might become the standard of care in the future.
The pace of innovation demands continuous learning and adaptation. Staying abreast of the latest advancements is not just an academic endeavor; it's a commitment to ushering in a new dawn in cancer treatment. Every breakthrough, every refined protocol, and every successful clinical trial inch us closer to a world where cancer's menacing shadow is considerably diminished, offering hope and renewed life to countless individuals worldwide.
Want to read more about new advances in immuno-oncology and ongoing immune therapies? Sign up to our Immuno newsletter to receive leading experts opinions, research and cutting-edge presentations on the latest advancements in cancer immunotherapy, with dedicated sessions on different therapeutic modalities as well as case studies on innovative preclinical and translational tools.