Exploring Oncology Biomarkers in Early Clinical Trials and Precision Medicine: Challenges and Opportunities

Biomarkers play a crucial role in the field of translational oncology, aiding in patient selection and treatment monitoring in early phase I clinical studies and beyond. However, identifying the right biomarker and understanding its significance can be a complex task. This article discusses insights from a panel discussion at Oxford Global’s Immuno & Biomarkers US conference. The discussion featured experts in the field, highlighting the challenges and opportunities associated with biomarker research in early clinical trials.
RELATED:
- A ‘New Age’ of Biomarker Technology? Understanding Identification & Validation of IO Biomarkers
- Improving Patient Response Through Effective Biomarker Development
- Three Leading Perspectives on Biomarker Diagnostic Discovery in Immuno-oncology
Moderating the discussion was Michael Damore, Director, and Translational Oncology Lead at Pfizer. Damore works almost exclusively in early phase I clinical studies involving biomarkers and pharmacodynamics. His areas of focus are determining when a drug candidate hits its target and patient selection for clinical trials. Damore said that his biggest challenge was in coming up with the right biomarker and then the subsequent analysis of blood and biopsy.
Also joining the panel was Kenneth Ramos, Executive Director, Texas A&M Institute of Biosciences and Technology. Ramos’s expertise lies in integrative genomic medicine and the rolling out of the precision medicine initiatives in Arizona and Texas.
Liling Warren, Senior Director and Head of Translational Statistics at Teva Pharmaceuticals, rounded the panel out. Warren is a statistician by training and said her biggest challenge was in looking for robust blood based biomarkers with an emphasis on accuracy, sensitivity, specificity, and clinical applicability.
P-Values in Early Phase Trials
Warren kicked off the discussion with the topic of using P-values as a metric for ranking biomarker candidates in the early phases of clinical trials. She said that often, in these early phases, the cohort size is just not large enough to generate a meaningful P-value to challenge a hypothesis. As a result, Warren recommended keeping replication in mind instead of worrying about the P-value at this early stage. “In these cases, worry about validating the hypothesis,” said Warren.
Therefore, when making the call for patient selection in phase II, Warren added that it is critical to make sure that the biomarker under investigation is a meaningful one. “At that point, you are still generating your hypotheses, but if you use prior experiments in the discovery phase in conjunction with historical public and control data, that can help strengthen your hypothesis.”
LINE1 Biomarkers
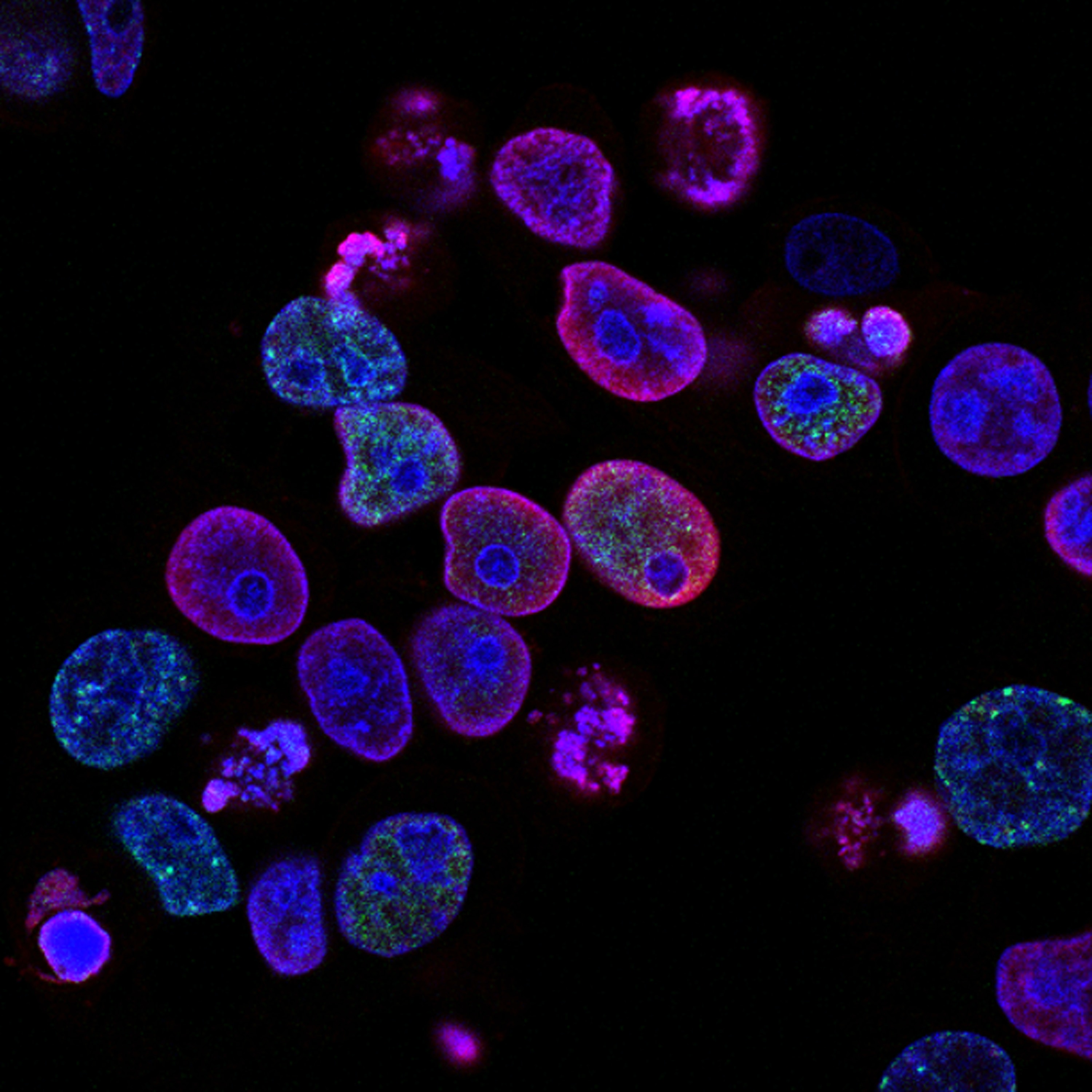
Later in the conference, Ramos went on to discuss his approach to using LINE1 (long interspersed nuclear element 1) as a biomarker for lung cancers. Here in the panel, he highlighted an overview of this approach. He noted: “LINEs are present in quite a few different tumours – breast, colon, GI, and lung cancers have particularly high levels.”
Ramos added that the lung was a preferred tissue for reactivation of those elements which function as transposable elements or ‘jumping genes’ – sequences that hop from one section of the genome to another. “They are involved in genomic instability, insertional mutagenesis, and tumour progression. Furthermore, they can activate oncogenic signalling which can give rise to highly malignant invasive tumours.” Ramos and his team have been probing LINE1 biology and using a liquid biopsy platform to create a mechanism-based biomarker.
Biomarkers Across the Progression of Cancer
Damore asked Ramos whether it was common to see a change in LINE1 biology from the first presentation of the cancer to later manifestations or metastases. “We certainly do,” confirmed Ramos. One approach that his team have taken has been to move away from observations of cancer patients themselves, and instead looking at pre-neoplastic states for lung cancer susceptibility and following their trajectory.
“One of the most difficult things for biomarker work is if you’re looking at cancer only, you don’t know if the mutations you see are passenger or driving mutations,” explained Ramos. One approach that his team has employed has been to evaluate chronic obstructive pulmonary disease patients, many of whom are at heightened risk of malignant progression, and then track the progression of a biomarker longitudinally from pre-neoplastic states into a cancer stage.
Ramos noted that elevations in LINE1 are mostly seen early in the transition from pre-neoplasia into malignancy , before a very quick drop-off in the latter stages of malignancy – “we of course have all sorts of theories as to why this is.”
Biomarkers in Early Screening
Damore then brought up the question of when the most optimal timeframe for the introduction of screening biomarker work in clinical trials is. “We are always told by our clinical leads that physicians always want to be doing precision medicine, and they want a biomarker even in phase I. Do we really want to see biomarker work applied in early screening?”
Ramos agreed with this concern: “it is not wise to put all your stock into a single biomarker.” However, he noted that pairing up a useful biomarker with other biomarkers and other technologies was a powerful way to conduct screening. “In cases of lung cancer, there is a huge advantage in that you’ve got low dose CT screening which is now being increasingly used to identify patients at risk – with nodules that you can follow up longitudinally,” said Ramos. Therefore, pairing a low dose CT with a biomarker will lead to superior sensitivity and specificity.
With regards to biomarkers applied to early screening, Ramos said he was in favour of this approach. He said: “from my perspective, the answer is yes. The reason that I say that is because the most useful tool that precision medicine gives you is the stratification of populations.” Biomarkers allow for said stratification which, in turn, enables better targeting of clinical endpoints.
Damore agreed with this point, but warned that especially in phase I, clinicians should be careful that they are not chasing prognostic biomarkers: “Because we don’t have a control, we can’t ensure that all subjects regardless of the therapy will respond better.”
What’s Next?
Biomarkers hold immense potential in early clinical trials, aiding in patient selection, treatment monitoring, and stratification of populations. However, the challenges associated with identifying the right biomarkers and understanding their significance remain significant.
Collaborations between researchers, pharmaceutical companies, and technology providers are crucial to overcoming these challenges and advancing the field of translational oncology. By adopting a multi-dimensional approach and combining biomarkers with other diagnostic tools, precision medicine can continue to improve patient outcomes and transform cancer care.
Join our two-day Immuno event packed with leading speakers, research and cutting-edge presentations on the latest advancements in cancer immunotherapy, with dedicated sessions o n different therapeutic modalities as well as case studies on innovative preclinical and translational tools.