Balancing Innovation and Ethics: The Role of Regulation in Microbiome-Based Precision Oncology
Microbiome-based precision oncology is an emerging field that holds great promise in revolutionizing cancer treatment. The human microbiome, which consists of trillions of microorganisms residing in and on our bodies, has been found to play a crucial role in our overall health and well-being. Recent research has shown that the composition of the microbiome can impact the efficacy of cancer treatments. This article explores the intricate relationship between the microbiome and cancer treatment outcomes, delves into the ethical considerations of this innovative approach, and discusses the need for regulation in microbiome-based precision oncology.
Understanding the Role of the Microbiome in Cancer Treatment Efficacy
Gut bacteria, a key component of the microbiome, have been found to influence the effectiveness of cancer treatments. Studies have shown that certain bacteria can enhance the response to chemotherapy, while others may contribute to drug resistance. The presence or absence of specific bacteria can alter the metabolism and absorption of medications, affecting their distribution and therapeutic effects. Understanding the complex interplay between gut bacteria and cancer treatment is crucial for developing personalized treatment strategies in precision oncology.
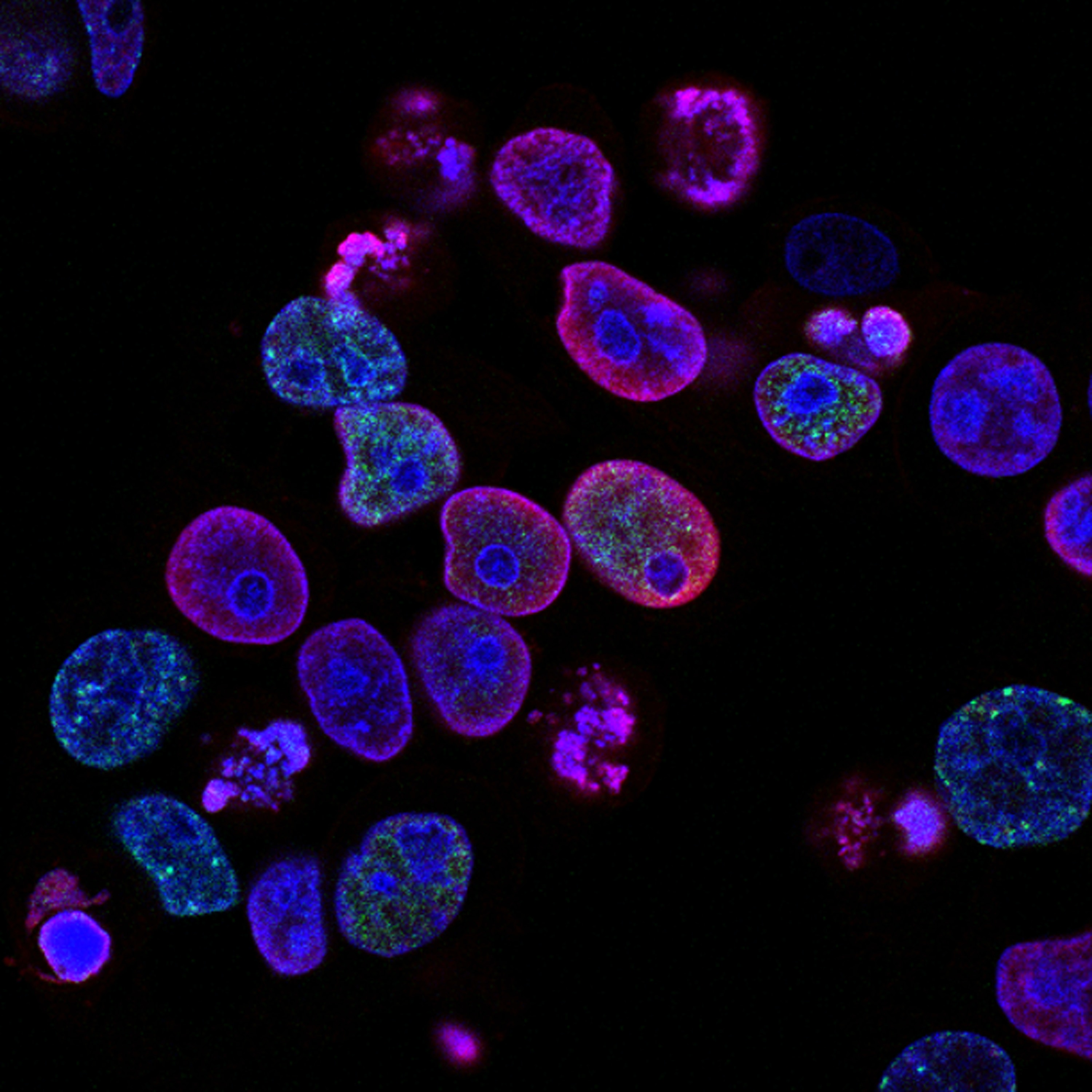
Furthermore, the microbiome has been linked to the efficacy of immunotherapy, a groundbreaking approach that harnesses the body's immune system to fight cancer. Research has shown that gut bacteria can modulate the response to immunotherapy by influencing the activation of immune cells and the production of certain molecules. By manipulating the composition of the microbiome, scientists hope to enhance the effectiveness of immunotherapy and improve patient outcomes.
The Impact of Gut Bacteria on Cancer Treatment Outcomes
The composition of the gut microbiome has been found to have a significant impact on cancer treatment outcomes. In a study published in Science, researchers found that patients with a diverse microbiome had better responses to immunotherapy compared to those with a less diverse microbiome. The presence of certain bacteria, such as Bacteroides species, was associated with increased tumor regression and prolonged survival. On the other hand, some bacteria, such as Akkermansia muciniphila, were found to be detrimental to immunotherapy response.
Similarly, the gut microbiome has been implicated in the response to chemotherapy. A study published in Nature Communications demonstrated that specific gut bacteria can metabolize chemotherapeutic drugs, either enhancing their efficacy or leading to drug resistance. The presence of certain bacteria, such as Firmicutes, was associated with improved response to chemotherapy, while others, such as Enterococcus hirae, were linked to drug resistance. These findings highlight the importance of considering the patient's microbiome when designing cancer treatment regimens.
Microbiome Research in Immunotherapy
The emerging field of microbiome research in immunotherapy is shedding light on the intricate relationship between the gut microbiome and the immune system. Studies have shown that specific bacteria can modulate the response to immunotherapy by activating immune cells and influencing the production of immune-regulatory molecules. For example, certain bacteria promote the accumulation of immune cells within tumors, leading to enhanced anti-tumor immune responses. Other bacteria can stimulate the production of molecules that suppress the immune system, dampening the effectiveness of immunotherapy.
Understanding the mechanisms underlying the interaction between the microbiome and the immune system is crucial for developing novel therapeutic strategies. Researchers are exploring various approaches, including fecal microbiota transplantation (FMT) and the use of probiotics, to manipulate the composition of the microbiome and enhance the efficacy of immunotherapy. However, ethical considerations must be taken into account when conducting microbiome research and implementing these approaches in clinical practice.
The Ethical Considerations of Microbiome-Based Precision Oncology
As with any innovative approach in medicine, microbiome-based precision oncology raises important ethical considerations. The manipulation of the microbiome through interventions such as FMT and probiotics raises concerns about safety, efficacy, and long-term effects. There is a need for robust clinical trials to evaluate the risks and benefits of these interventions, ensuring that patients are not subjected to unnecessary harm.
Furthermore, the potential for commercialization and profit in microbiome-based precision oncology raises questions about equity and access to these innovative treatments. Will these therapies be available to all patients, regardless of their socioeconomic status? How will the cost of these treatments be managed, and who will bear the financial burden? Ethical frameworks must be established to address these issues and ensure equitable access to microbiome-based precision oncology.
The Need for Regulation in Microbiome-Based Precision Oncology
Given the potential impact of microbiome-based precision oncology on patient care, it is essential to establish clear regulations and guidelines in this field. Regulation can ensure that interventions involving the manipulation of the microbiome are conducted ethically, with proper consideration for patient safety and privacy. Additionally, regulation can help prevent the dissemination of false or misleading information about microbiome-based treatments, protecting patients from unsubstantiated claims and potential harm.
Regulatory bodies, such as the Food and Drug Administration (FDA), play a crucial role in overseeing the development and approval of microbiome-based therapies. They assess the safety and efficacy of these interventions, ensuring that they meet rigorous scientific standards before being made available to patients. Collaboration between regulatory agencies, researchers, and healthcare professionals is essential to strike a balance between innovation and ethical considerations in microbiome-based precision oncology.
Current Regulations and Guidelines in Microbiome Research
At present, regulations and guidelines in microbiome research are still evolving. The FDA has issued guidance documents for the development of microbiome-based therapies, outlining the regulatory pathway for these innovative treatments. These guidelines emphasize the need for rigorous clinical trials to demonstrate safety and efficacy, as well as the importance of collecting long-term follow-up data to assess the impact of these interventions on patient outcomes.
Additionally, professional societies and organizations are developing guidelines to ensure the ethical conduct of microbiome research. These guidelines cover aspects such as informed consent, privacy protection, and data sharing. They aim to safeguard the rights and well-being of research participants while promoting scientific integrity and transparency.
Balancing Innovation and Ethics in Microbiome-Based Precision Oncology
Balancing innovation and ethics in microbiome-based precision oncology is a complex task. On one hand, there is a pressing need to advance scientific knowledge and develop novel therapies that can benefit patients. On the other hand, ethical considerations, such as patient safety, privacy, and equitable access, must be prioritized to ensure that the potential benefits of these therapies are realized without causing harm or exacerbating existing health disparities.
To achieve this balance, collaboration between researchers, healthcare professionals, regulatory bodies, and ethical experts is crucial. Open dialogue and transparency are needed to address the ethical challenges posed by microbiome-based precision oncology. Ethical frameworks should be developed to guide researchers and clinicians in conducting responsible and patient-centered microbiome research. Furthermore, public engagement and education are essential to ensure that patients and the wider community are informed about the potential benefits and risks of microbiome-based therapies.
The Future of Regulation in Microbiome-Based Precision Oncology
As the field of microbiome-based precision oncology continues to advance, the need for regulation will become increasingly important. The development of robust regulatory frameworks will help streamline the translation of research findings into safe and effective therapies. It will also address the ethical considerations surrounding the commercialization and access to these novel treatments.
Furthermore, ongoing research is needed to better understand the long-term effects of microbiome-based interventions and to identify potential risks and benefits. This knowledge will inform the development of evidence-based regulations that prioritize patient safety and well-being.
Conclusion
Microbiome-based precision oncology holds great promise in transforming cancer treatment. The complex relationship between the microbiome and cancer treatment outcomes necessitates a careful balance between innovation and ethics. Regulation plays a critical role in ensuring the safe and responsible development of microbiome-based therapies. By establishing clear guidelines and fostering collaboration among stakeholders, we can harness the potential of microbiome-based precision oncology while safeguarding patient safety and ensuring equitable access to these innovative treatments.
Don't miss out on upcoming immuno events! Stay informed and connected with our community by subscribing to our newsletter. Receive event updates, expert insights, and more








