Zika Virus Tested as an Effective Oncolytic Agent for Glioblastoma in In Vitro Models
Oxford Global previously reported the use of Zika virus at Nemours Children's Hospital as an oncolytic therapy for neuroblastoma, an extra-cranial nerve cell cancer. But the oncolytic properties of the virus are not limited to this indication, as scientists at Duke-NUS Medical School, Singapore, have used Zika to kill glioblastoma tumour cells and inhibit cancer growth.
The team used the virus, which is known to cause neonatal complications when contracted during pregnancy, as a cancer vaccine which targeted fast-growing cancer cells in the brain.
RELATED:
- In Vivo Models Show Survival Promise for Zika Oncolytic Viral Therapy for Neuroblastoma
- Immunostimulatory Oncolytic Viruses: Interview with Angelica Loskog, CEO, Lokon Pharma
- Positive Phase I Data from Oncolytic Virotherapy Trial
Senior Author, and Assistant Professor at Duke-NUS, Dr Ann-Marie Chacko said: "Since the Zika virus outbreak in 2016, understandably, there has been fear about the nature of the virus and its devastating effects. Through our work, we hope to present the Zika virus in a new light by highlighting its potential to kill cancer cells."
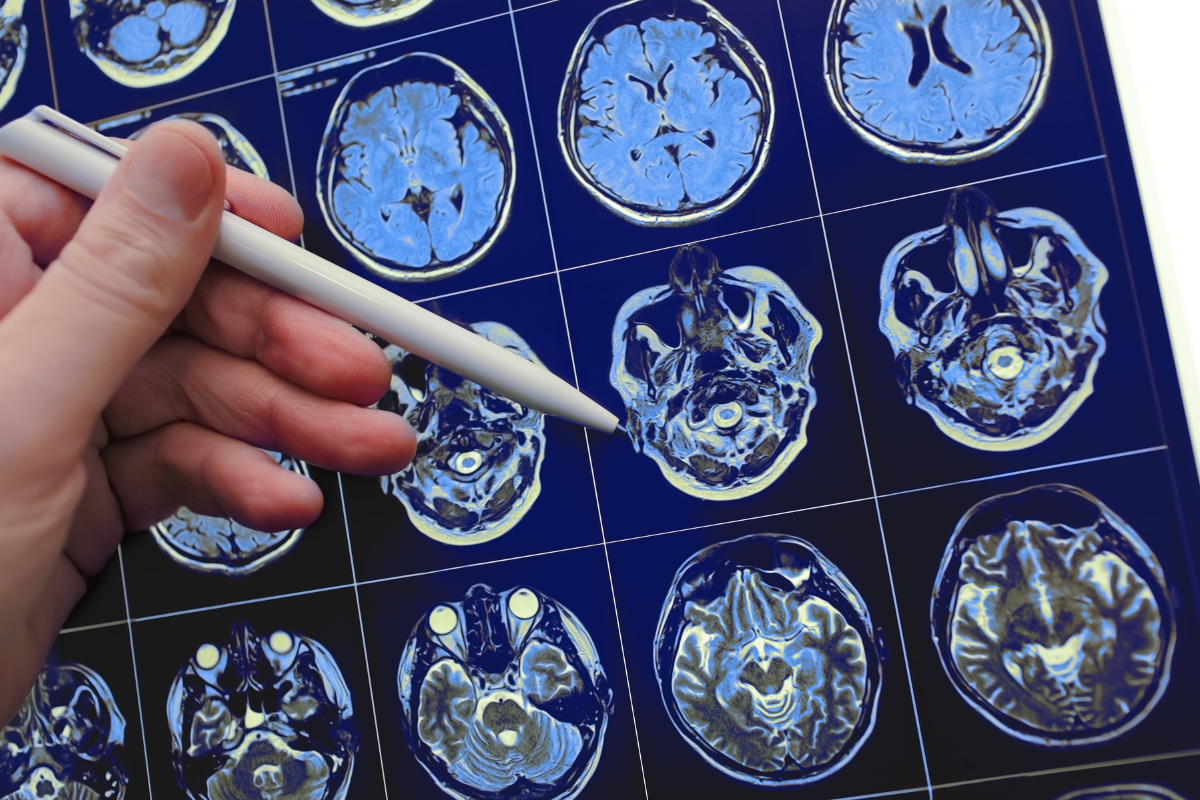
Glioblastoma is the most common type of brain cancer, its rapid-growing, highly-invasive, has poor prognosis (average 10-13 month survival rate after diagnosis), and few treatment options. The findings, which were published in the Journal of Translational Medicine, hope to change the treatment landscape of the disease.
The Duke-NUS team used 'weakened' strains of Zika that are less able to infect healthy cells called Zika virus live-attenuated vaccine (ZIKV-LAV). The virus can infect tumour cells however, where it creates copies of itself within the cell wall which ruptures (cell lysis), spreading Zika to other cells in the tumour mass.
"We selected Zika virus because it naturally infects rapidly multiplying cells in the brain, allowing us to reach cancer cells that are traditionally difficult to target. Our ZIKV-LAV strains also replicate themselves in brain cancer cells, making this a living therapy that can spread and attack neighbouring diseased cells," said Dr. Carla Bianca Luena Victorio, Senior Research Fellow at the Cancer & Stem Cell Biology Programme at Duke-NUS.
Dr. Victorio, who is the first author of the paper, and her team used the cancer vaccine candidate against human glioblastoma cells in vitro. Auspicious results were seen in cancer cells that were infected by ZIKV-LAV – 65 to 90% of the cells died from the therapy. Furthermore, although the virus did infect some healthy blood vessels in the brain, these cells were spared from lysis, proving the efficacy of the group's 'weakened' strain.
"When a live virus is attenuated, such that it is safe and effective to fight infectious diseases, it can be beneficial to human health—not just as a vaccine but also as a potent tumour-eradicating agent," said Dr. Chacko.
The results from this in vivo experiment, combined with the positive in vitro data at Nemours, promote further hope for the oncolytic effect of Zika. Next, the team want to translate the therapeutic mechanism of the virus to other cancers and further improve its safety profile.
Professor Patrick Tan, Duke-NUS's Senior Vice-Dean for Research, commented: “This is a sterling example of how different research programmes within the School come together to tap their various expertise to advance medical knowledge and improve patients’ lives. The team’s valuable insights may one day translate into a new treatment option to control tumour growth or even, offer a cure for cancer.”






