Developing Novel Theranostic Approaches for the Development of Oncolytic Viruses
Transcribed by Tom Cohen.
Developing Oncolytic Viruses
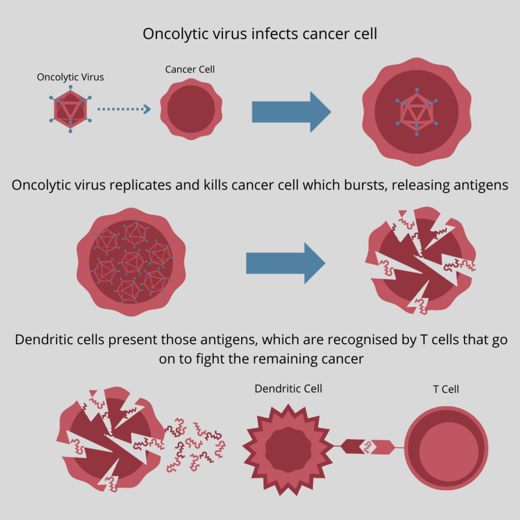
Oncolytic viruses are naturally or specially designed to infect and kill cancer cells. The cell death that occurs as a result can trigger an adaptive immune response, which in-turn, helps destroy the cancer on a larger scale. This novel method of immunotherapy is fast approaching the forefront of modern medicine, but its future success will be dependent on the capacity to understand the virus’s efficacy and replication in living cells.
Dr Pierre Cordelier is an INSERM (French National Institute of Health and Research) Research Scientist for The Cancer Research Centre of Toulouse (CRCT) and works on moving oncolytic viruses into the clinical phase of development. They have a close connection to the clinics in the CRCT that process samples from patients with cancer, and with the company NeoVirTech which develops imaging and screening for viral and antiviral therapies.
Dr Cordelier explained at Oxford Global’s Preclinical Immuno-Oncology: Online 2022 that the main challenge for developing oncolytic viruses is that viral dynamics and efficacy are hard to capture. Furthermore, he says that because of this, new technologies are needed to bridge this gap in capability.
NeoVirTech detect viral DNA in living cells and have developed a system which they call ANCHOR to do so. A DNA sequence referred to as ‘ANCH’ is inserted into the genome of a virus’s DNA, which encodes for the expression cassette of a protein they call ‘OR’. The OR protein can be fused with a fluorescent protein so once it is produced in the cell, fluorescent imaging of the ANCH sequence can be performed and viral replisomes are easy to spot.
Dr Cordelier’s lab applies this technology to be used in oncolytic viruses, “we are able to track the early, advanced, and late stages of infection in live cells.” This made them able to monitor the time for full-replication, cell-to-cell propagation, and cell death, leaving them with a better understanding of virus kinetics in those cells.
“Interestingly, increasing the multiplicity of infection (MOI) only shortened the time for cell-to-cell propagation,” said Dr Cordelier, “an interesting insight into the biology of oncolytic viruses in primary cells.”
“Quantitative, Real Time, Longitudinal Studies”
The CRCT has been able to develop a series of “quantitative, real time, longitudinal studies on cancer cells that are infected for a long period of time.” Using live cell imaging, the research team were able to quantify the inner workings of those cells and identify which are resistant, which are semi permissive, and which are fully permissive: “This is useful when you want to stratify patients.”
“Of course, we want to move this modelling into the third dimension,” said Dr Cordelier, outlining how the CRCT is utilizing spheroids and organoids for their project: “If you want to set up a preclinical platform to test your molecule of interest (here it’s a virus) you need to provide the patient-derived resources in a timeframe that is compatible with therapeutic decisions — and organoids do great with that.”
- Improving Preclinical Modelling for IO
- Challenges in Developing Organoids for Neuroscience
- Experts Discuss Next Generation Organoids: Challenges and the Future
One step further into the 3D resolution of virus infection is combining the ANCHOR system with light-sheet imaging. NeoVirTech, with the help of Imactiv3D imaging facilities, trialled this by infecting cancer cells with a VacV ANCHOR Santaka encoded virus. “Reconstitution in 3D gives you a good understanding of how deep the virus goes,” says Dr Cordelier, they managed to find that 94% of the cancer was infected with the virus.
This can also help you determine which combination can improve or shut down viral infection in cancer cells. “It is pretty clear that you need a second or third hit to try to promote the virus infection or drug sensitivity to try to eradicate cancer cells — especially in pancreatic cancer.” The system is compatible with high throughput screening of over 1,200 samples which can then be analysed thanks to the ANCHOR system: “From that you can identify combinations to improve or shut down viral infection.”
Cordelier’s lab is providing biological data on confluence, viral replication, and cell cycle following infection. From these data they can model infection with colleagues that are computer scientists, and, as Dr Cordelier explains, they can control many parameters in those models including number of replications after the primary infection and time of replication. “This helps us better understand the biology of oncolytic infection in cancer cells,” says Dr Cordelier.
“Running this simulation thousands of times with our colleague Dr. Sylvain Cussat-Blanc provides us with the best possible outcome.” Cordelier stated that by tweaking the parameters, they can optimise the virus to lower the risk of resistance — so far this have proved successful with 95% effectiveness: “By optimising the dose and time of infection, the virus’s population growth will be such that you eliminate relapse.”
“Are We There Yet?”
Dr. Cordelier’s final thoughts addressed the question that crosses every researcher’s mind: “are we there yet?” The good news, as Dr. Cordelier explained, is that there are many ongoing trials for oncolytic viruses, “but we still have to work towards precision medicine in this field.”
“I think that this strategy will help better define preclinical platforms to address OV efficacy,” concluded Dr. Cordelier, adding that: “We will also better identify combinations to help improve or shut down infections, and with our modelling strategy, better define the dose and the timing — including in combination with therapies.” It is the hope of Dr. Cordelier and his team within the CRCT that this will be the next, most crucial step towards ‘rationally designed virotherapy trials for cancer management, in close collaboration with clinicians from the Toulouse Oncopole hospital.
Join Immuno UK: In-Person for valuable insights into the approaches impacting the immunotherapy field through 40+ outstanding presentations tackling key discussion points in immuno-oncology, immunology, and inflammation.