How to Improve Therapeutic Efficacy: Safety Considerations in Oncolytic Virotherapy
Oncolytic virotherapy, a approach in cancer treatment, utilizes viruses to selectively infect and destroy cancer cells. This field of research has shown immense promise in enhancing therapeutic efficacy while minimizing the side effects associated with conventional cancer treatments. By leveraging the natural ability of viruses to replicate within cells, oncolytic virotherapy offers a targeted and personalized approach to cancer treatment.
What is Therapeutic Efficacy of Oncolytic Viruses?
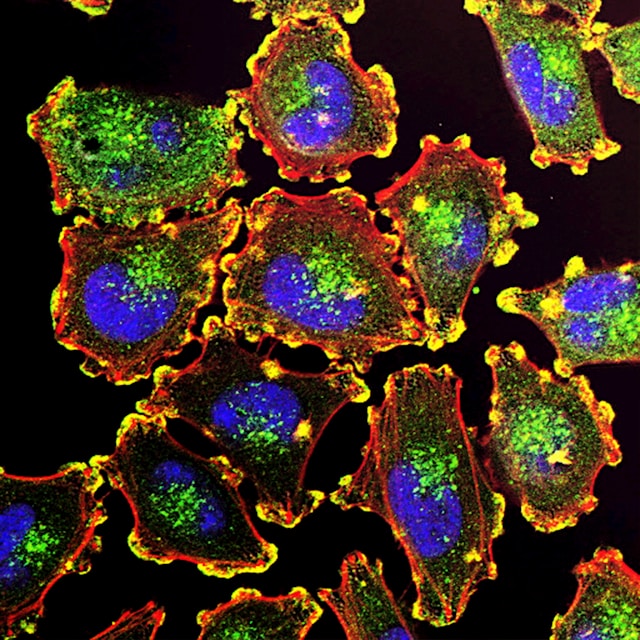
The therapeutic efficacy of oncolytic viruses lies in their ability to preferentially infect and replicate within cancer cells. Oncolytic viruses are engineered to exploit the unique vulnerabilities of cancer cells, such as dysregulated signalling pathways or deficiencies in antiviral defence mechanisms. Once inside the cancer cells, these viruses replicate and cause lysis, leading to the destruction of the tumour. Additionally, the infection triggers an immune response, further aiding in the elimination of cancer cells.
Recent studies have highlighted the potential of oncolytic viruses to enhance therapeutic efficacy through multiple mechanisms. Firstly, the direct killing of cancer cells by viral replication and lysis reduces the tumor burden. Secondly, the release of tumour-associated antigens during viral replication stimulates an immune response, leading to the destruction of both infected and non-infected cancer cells. Lastly, oncolytic viruses can be engineered to express therapeutic genes, allowing for targeted delivery of therapeutic payloads to the tumour microenvironment.
What are the Safety Considerations in Oncolytic Virotherapy?
While oncolytic virotherapy holds tremendous potential, safety considerations are paramount to ensure patient well-being. As with any therapeutic intervention, minimizing adverse effects is crucial. One primary concern is the potential for viral replication in healthy cells, leading to unintended damage. To mitigate this risk, researchers have focused on modifying the viral genome to restrict replication to cancer cells while sparing normal tissues. Additionally, stringent preclinical testing is essential to evaluate the safety profile of oncolytic viruses before advancing to clinical trials.
Another safety consideration is the potential for systemic viral dissemination, which could result in widespread infection. Researchers employ various strategies to address this concern, including the use of tumour-targeting ligands or encapsulation within vehicles that selectively deliver the oncolytic viruses to the tumour site. Furthermore, monitoring and managing the immune response to the viral infection is crucial to prevent excessive inflammation or autoimmune reactions.
What are the Challenges and Limitations of Oncolytic Virotherapy?
Despite the promising results observed in preclinical and early clinical studies, oncolytic virotherapy faces several challenges and limitations. One major hurdle is the development of resistance to viral infection within cancer cells. Cancer cells can evolve mechanisms to evade viral infection, thereby reducing the effectiveness of oncolytic virotherapy. Researchers are actively investigating ways to overcome this resistance, such as combining oncolytic viruses with other therapeutic modalities, including immunotherapy.
Another limitation is the potential for off-target effects, where the virus may inadvertently infect normal cells or healthy tissues. This can result in adverse events and limit the therapeutic window. To address this, researchers are exploring novel strategies to enhance the specificity and selectivity of oncolytic viruses, such as genetic modifications or the use of viral vectors that target specific cell surface receptors.
Can you Combine Oncolytic Viruses with Immunotherapy?
Immunotherapy has revolutionized cancer treatment by harnessing the power of the immune system to recognize and eliminate cancer cells. Combining immunotherapy with oncolytic virotherapy has emerged as a promising approach to enhance therapeutic efficacy. Oncolytic viruses can serve as potent immune stimulators, triggering immune responses that not only target infected cancer cells but also provide long-term protection against tumour recurrence.
One approach is to engineer oncolytic viruses to express immunomodulatory molecules, such as cytokines or immune checkpoint inhibitors, which enhance the immune response against the tumour. Additionally, oncolytic viruses can be used in combination with immune checkpoint inhibitors to overcome the immunosuppressive microenvironment within tumours, allowing for more robust antitumor immune responses. These combination therapies hold great potential for improving patient outcomes and expanding the applications of oncolytic virotherapy.
Immune Responses to Oncolytic Viruses
The immune response elicited by oncolytic viruses plays a pivotal role in their therapeutic efficacy. Upon viral infection, the immune system recognizes the viral antigens expressed on infected cancer cells, leading to the activation of both innate and adaptive immune responses. The innate immune response, involving natural killer cells and macrophages, contributes to the initial antitumor effects by direct killing of infected cells and the release of pro-inflammatory cytokines.
The adaptive immune response, mediated by T cells and B cells, provides long-term protection against tumour recurrence. Tumour-specific T cells are activated and expanded upon exposure to viral antigens, leading to the destruction of both infected and non-infected cancer cells. The memory T cells generated during this process can recognize and eliminate tumour cells even after viral clearance.
Strategies to Enhance the Safety of Oncolytic Virotherapy
To enhance the safety profile of oncolytic virotherapy, researchers are developing strategies to minimize off-target effects and improve the specificity of viral replication.
- Modifying the Viral Genome
This approach involves modifying the viral genome to restrict replication to cancer cells, either by targeting specific signalling pathways or relying on the unique characteristics of the tumour microenvironment. By engineering the viruses to have a limited host range, researchers aim to minimize the risk of infecting healthy cells.
- Prodrug-Converting Enzymes
Another strategy is the use of prodrug-converting enzymes, which are expressed by the oncolytic viruses within the tumour microenvironment. These enzymes convert non-toxic prodrugs into potent cytotoxic agents, resulting in localized tumour cell death. This approach allows for a more targeted and controlled therapeutic effect, reducing the risk of off-target toxicity.
Clinical Trials and Advancements in Oncolytic Virotherapy
The field of oncolytic virotherapy has witnessed significant advancements in recent years, with numerous clinical trials underway to evaluate the safety and efficacy of various oncolytic viruses. These trials aim to establish the optimal dosing, delivery methods, and combination therapies to maximize therapeutic outcomes. Additionally, advancements in viral engineering techniques and the development of novel viral vectors have expanded the repertoire of oncolytic viruses available for clinical use.
Several oncolytic viruses have already received regulatory approval for the treatment of certain types of cancer. For example, T-VEC (talimogene laherparepvec) has been approved for the treatment of advanced melanoma. As further clinical data emerges, oncolytic virotherapy is expected to become an integral part of the cancer treatment armamentarium, offering new hope for patients with limited treatment options.
Future Prospects and Potential Applications of Oncolytic Virotherapy
The future of oncolytic virotherapy holds immense promise, with potential applications beyond the treatment of primary tumours. Researchers are exploring the use of oncolytic viruses for the treatment of metastatic disease, where the viruses can target and eliminate cancer cells that have spread to distant sites. Additionally, the combination of oncolytic virotherapy with other emerging therapeutic modalities, such as gene therapies or targeted therapies, may further enhance treatment outcomes.
Furthermore, the field of oncolytic virotherapy is evolving to address the challenges and limitations encountered thus far. Ongoing research aims to optimize viral engineering techniques, improve viral delivery methods, and develop innovative strategies to overcome resistance mechanisms. These advancements will pave the way for more effective and personalized cancer treatments, bringing us closer to the goal of eradicating cancer.
Conclusion
The therapeutic efficacy of oncolytic viruses lies in their ability to target and eliminate cancer cells while stimulating an immune response against the tumour. However, safety considerations are paramount to ensure patient well-being, and researchers are actively working to enhance the safety profile of oncolytic virotherapy.
Combining oncolytic viruses with immunotherapy has emerged as a promising strategy to enhance therapeutic efficacy and overcome the limitations of oncolytic virotherapy. The immune response elicited by oncolytic viruses plays a crucial role in their antitumor effects, and strategies to enhance immune activation are being explored.
As clinical trials progress and advancements continue, oncolytic virotherapy is expected to revolutionize cancer treatment and expand the treatment options available to patients. The prospects of oncolytic virotherapy are bright, with potential applications in metastatic disease and in combination with other emerging therapeutic modalities.







