Improving Patient Response Through Effective Biomarker Development

Oxford Global was delighted to welcome a distinguished panel of scientists to discuss strategies for biomarker development for immunology and immuno-oncology, as well as their impact on clinical trials. Joining the discussion from the panel were Matteo Cesaroni, Group Head, Precision Oncology, Bioinformatics at Sanofi; Petra Prinz, Director of Immunoprofiling at Medigene; and Gabriel Wong, Director of Discovery Medicine, Immunology at AstraZeneca.
Tracking Patient Response with Immune Profiling
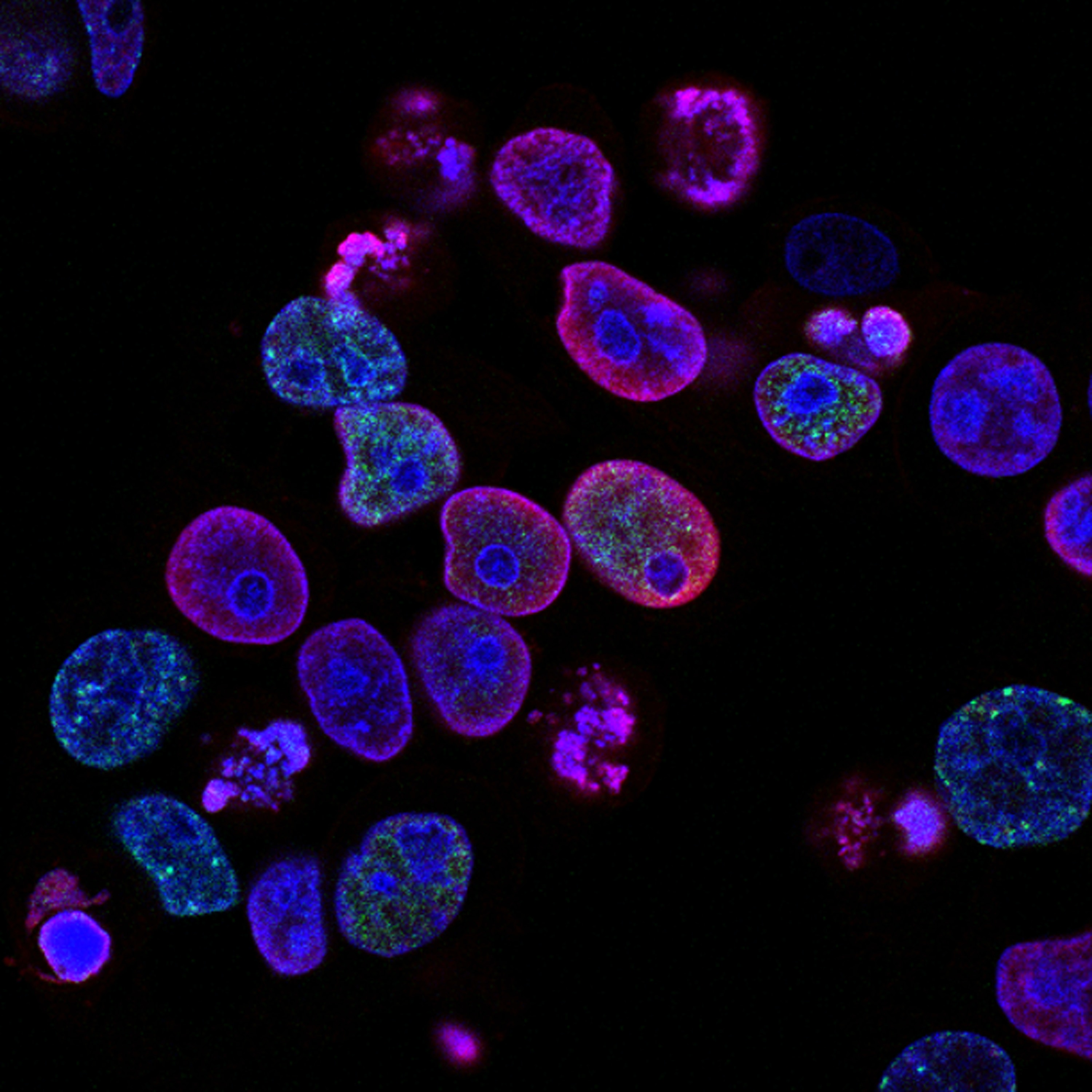
The panel were first asked how immune profiling was utilised to track patient response. Prinz is part of Medigene’s translational medicine group which is focussed on the characterisation of their TCR-T drug products. Prinz said that there was “intense characterisation phenotypically and functionally which we hope we can link to anti-tumour effects and clinical outcome.”
“There is a lot of room for improvement, especially with new technology that’s more innovative,” added Prinz. Technologies such as single cell analysis and spatial transcriptomics are among the forward thinking methods that Prinz would like to see improving the field.
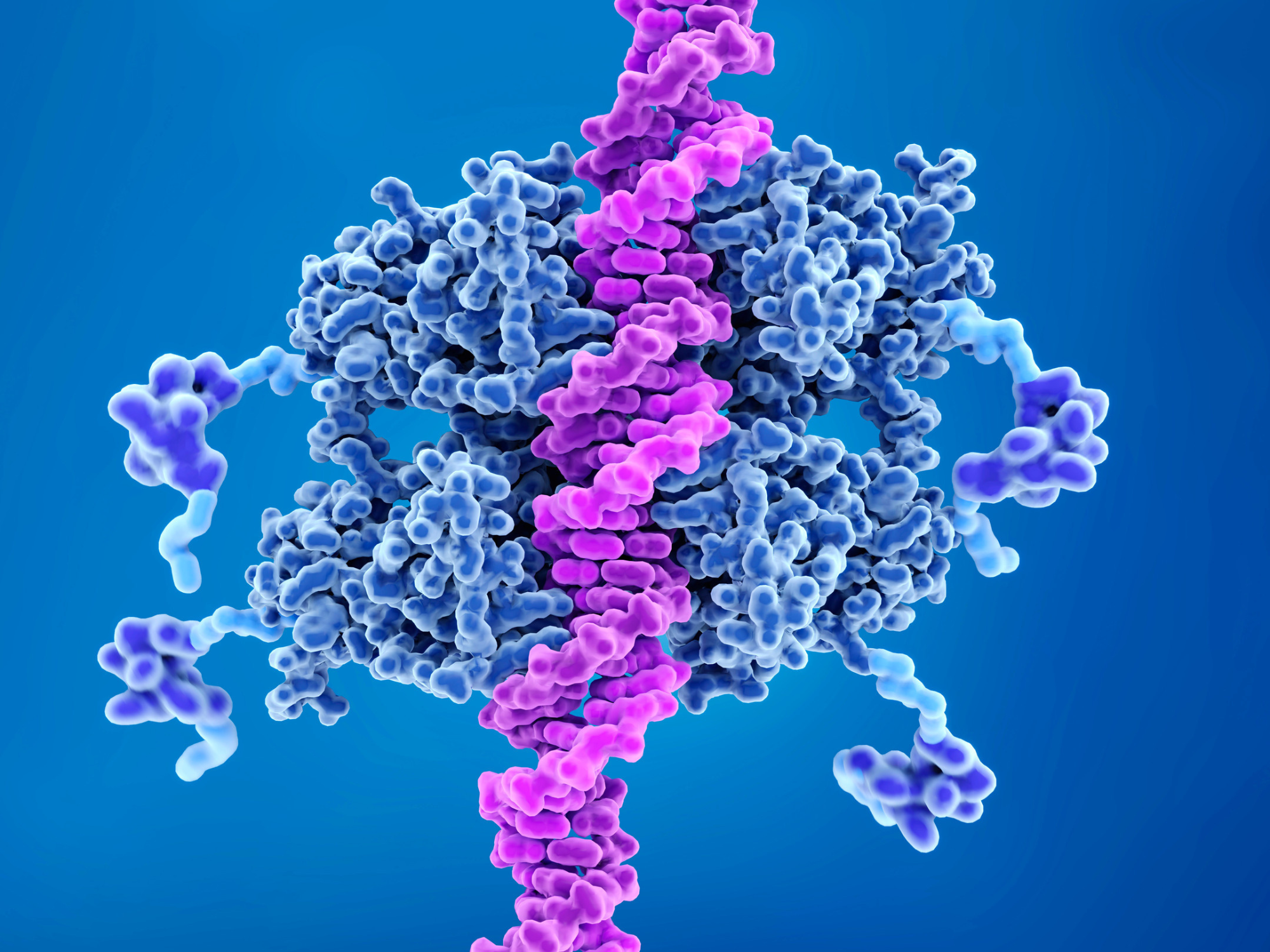
“At Sanofi, we start each program from the discovery phase,” said Cesaroni. “As soon as we have something interesting, be it a gene or a cell type, we start very early to put a biomarker plan on the table for developing a specific drug” he added.
Sanofi use a variety of technologies in order to discover biomarkers for a specific drug, such as single cell and spatial transcriptomics. Here they can look at gene signature, gene expression, and mutation.
- Three Leading Perspectives on Biomarker Diagnostic Discovery in Immuno-oncology
- Perfecting Precision Medicine: The Promise of Biomarkers and Spatial Biology
- Combination Therapies and Biomarkers – A Holy Grail for Improved IO Treatments
Cesaroni then introduced a key question: which biomarker can be used in the clinic? “If I need to do a single cell experiment for the patient, that’s not going to be possible,” he said. Here he stressed the importance of translating discovery biomarkers to something that is practical and usable in the clinic.
Wong came at this question from a different angle due to the fact that he works in autoimmunity and immunology rather than with cancer. “The challenge that we face is in stratifying patients based on one marker,” he explained. Clinicians working with autoimmune and inflammatory diseases don’t have the ability to stratify patients based on the binary of having a mutation or not like in the cancer field.
“Often, we work with a more graded response, even for one biomarker,” explained Wong. Therefore, one challenge for the autoimmune field is in identifying the cut-off point in deciding which biomarkers are relevant.
The technology to better characterise patients is also a desire for Wong, he said that having the information that those methods can provide would be very valuable to work with. “At the moment, we don’t have a cohesive way to actually collect samples together either nationally or locally,” Wong continued. Gathering enough information to understand the changes in biomarkers longitudinally will be a critical milestone as well.
The Timepoint of Acquiring Biomarkers for Longitudinal Study
The acquisition of biomarkers in longitudinal studies was mentioned by an audience member. In a controlled, pre-clinical setting there are a wide variety of biomarker options available, but in the clinic, it is a different story. In a clinical setting, scientists need to make sure that ‘the perfect biomarker’ coincides with the time that the patient visits the clinic.
The attendee asked the panel how they could engineer this upfront, especially when using tools like single cell sequencing and spatial transcriptomics where the timepoint is critical. “We know that the genes are switched on at different timepoints,” he added. “But how do we actually bridge the two?”
Wong was first to answer, he commented that it would be helpful to see more predictive biomarkers for patient response. Predictive biomarkers are different to response biomarkers which help understand how a therapy performs with clinical response at the time.
Predictive biomarkers help to anticipate the patient’s response to treatment. These biomarkers must be understood at the point of a patient’s enrolment in a clinical trial. Therefore, scientists may expect different biomarkers to highlight the disease stage at different time points.
The timeframe for measuring cancer biomarkers is a different story to autoimmune diseases. Cesaroni said that a CT scan might show that a tumour shrinks which is an objective measurement. But for autoimmune conditions, a clinician that sees a patient every two months will only have a good idea of their condition in two months’ time — missing out on all the data in between.
This is when Cesaroni introduced the concept of digital biomarkers, a powerful and ambitious new way of tracking disease. Wearable devices are used to track and store the data for digital biomarkers, making them very well suited for patient response to treatment for autoimmune diseases.
For patients with lupus or rheumatoid arthritis, their lifestyles can change drastically depending on whether they have a flare-up or not. Therefore, having continuous and remote monitoring of the patient’s activity can really change the life of the patient and their treatment.
Collaboration and Using Complex Biomarkers in Clinical Trials
Another question asked by an audience member concerned implementing and analysing biomarkers in phase I and II immuno-oncology studies. She had noticed in the transition from academia to industry that tests that are considered ‘easy’ in an academic setting can prove difficult in clinical trials. However, those more complex tests have nevertheless proved their worth, exemplified by the results of single cell RNA seq in studying checkpoint inhibitors. The audience member therefore suggested that collaborations with academic partners would be a way of mediating this difficulty.
Cesaroni pointed out that there had been some efforts to move in this direction, at least in immuno-oncology. He cited a consortium called IMMUcan which compiles samples from multiple hospitals, it includes bulk RNA seq and single cell data from hundreds of patients. “So, there are efforts to work together and start to collaborate.“ The challenge with this kind of collaboration is that it requires huge monetary investment.
The strategy that Cesaroni recommended was to start collaboration with multiple centres and try to harmonise the data together, after that the useful data can be extrapolated. “Then you can maybe come up with a biomarker that doesn’t require single cell analysis — but you need to generate this data first.”
But this creates a cyclical problem. Many scientists running clinical trials don’t want to ask their patients for up to three biopsies due to the fear of putting people off participating. Therefore, often the data required to discover easier biomarkers does not get generated.
For more insights into immuno-oncology, as well as commentaries, discussion group reports, and Q&As, sign up for our Immuno newsletter to receive monthly highlights. Are you interested in more about biomarkers in immuno-oncology? Why not come along to our next Immuno UK and Biomarkers UK conferences this year.