Immunology: from Cancer to COVID
Long COVID, Autoimmunity, and Cardiac Problems
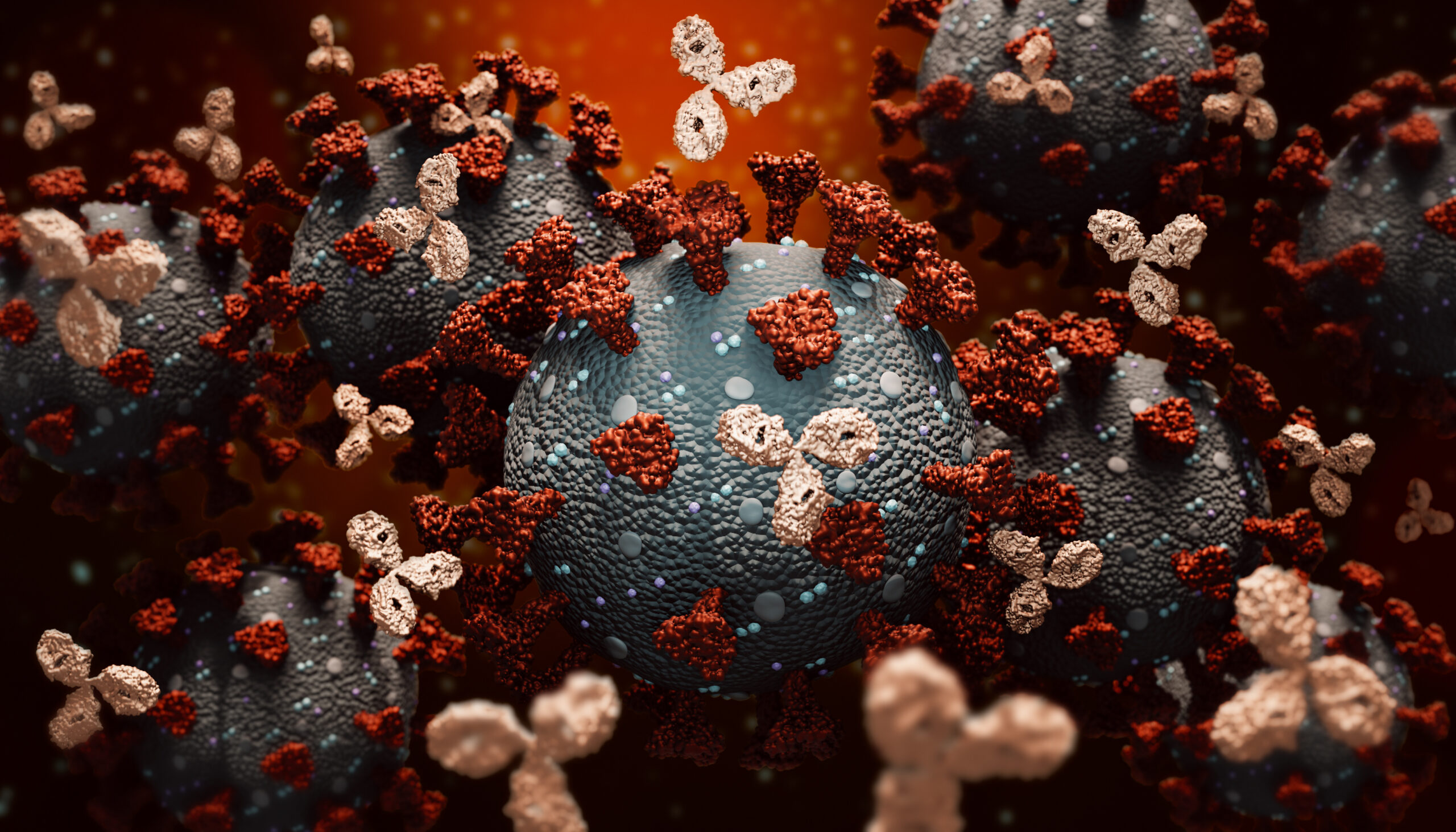
David Wraith is a Professor of Immunology and Director of the Institute of Immunology and Immunotherapy at University of Birmingham. Wraith began our panel discussion at Immuno UK 2022, titled Immunology: From Cancer To COVID-19, and said that at the beginning of the pandemic, he had embarked on a project to develop a sensitive antibody test for the COVID spike protein. “That led us to conduct a lot of studies, first in healthcare workers of different groupings – collecting a lot of samples,” he said.
“Frankly, the results were quite frightening”
When it was first becoming known that COVID-19 infection could cause long-term post-convalescent syndrome (widely known as long COVID), Wraith and his team decided to run routine clinical autoimmune marker assays on samples collected from patients. “Frankly, the results were quite frightening,” said Wraith.
They looked at the classic, clinically defined autoantibodies in these patients, most of whom had survived the ICU but then developed the long-term sequelae. About 75% of the individuals tested who were convalescent after COVID developed autoantibodies. “What was very interesting was the pattern of autoantibodies,” Wraith added. For example, there was a high instance of epithelial antibodies: “like how you would define bullous pemphigoid – but most of the patients in this group don’t have skin blistering or other symptoms consistent with that.”
- The Challenges Facing Antibody-Drug Conjugates for Immuno-Oncology
- Immuno Oncology Investigations: The NKG2D Pathway, Diagnostic Biomarker, and Allogenic CAR Ts
Furthermore, Wraith noted that a lot of these patients also had cardiac complications, so his team looked at staining patterns of heart tissue, and staining patterns of skin. “It looked as though the antibodies were staining what the pathologists call the intercellular cement,” explained Wraith.
They also looked for desmosomal proteins in the serum of patients with acute or convalescent COVID and found desmoplakin and desmoglein 2 (not 1 or 3), at high levels in the serum of these patients. “So, we reasoned that if there were proteins being released, then possibly there will be antibodies,” said Wraith.
Given this, Wraith’s team set up a desmoglein 2 screen and validated it. Wraith disclosed that “the patients had remarkably high levels of desmoglein 2 autoantibodies.” Evidence from experimental models shows that antibodies of this type can disrupt desmosomal structures in heart tissue. This effect was corroborated by post-mortem evidence of disrupted intercalated discs the hearts tissue in COVID mortalities.
Wraith said that “we don’t know yet whether there is a direct causal effect. But if there is, and this is a contributor to long-COVID, then there is something we can do about it.” He suggested the possibility of autoantibody removal: suppressing the inflammatory response arising from the impact of the antibodies to reinstate tolerance for these proteins. “So, I think this is a very challenging and potentially interesting area.”
Using Existing Therapeutics for New Targets
Also on the panel was Paul Eggleton, Professor & Senior Director of Immunology at Revolo Biotherapeutics, who discussed utilising existing therapeutics for new targets. Eggleton mentioned the fact that evidence suggests that patients with inflammatory bowel disease are at a greater risk of developing Parkinson’s disease. While at UCB, Eggleton and colleagues were interested in the large meta-analyses world-wide, studying if the treatment of IBD patients with an anti-TNF can protect some of these patients going on to develop Parkinson’s disease. “So, repurposing drugs originally used for cancer are sometimes useful to treat autoimmunity. It might also be true for repurposing drugs useful when treating inflammatory disease, that they in turn might be useful to reduce developing some neurodegenerative diseases,” Eggleton noted.
- Treating Autoimmune Diseases: Past, Present, and Future
- Re-Educating the Immune System: a ‘Brave New World’ in Immunology
Furthermore, Eggleton said that due to COVID, the repurposing of therapies had skyrocketed: “we’ve thrown everything at COVID.” He added that the process for repurposing drugs usually goes through an orderly long and regimented workflow of testing. However, in the COVID pandemic, due to the urgency, many tried and tested immunosuppressive drugs used routinely in humans were fast-tracked for repurposing to treat the inflammatory symptoms of COVID.
“There are numerous ‘named’ autoimmune diseases, but what I often tell medical students is they should probably think of all autoimmune diseases as just one pan-autoimmune disease. Many pro-inflammatory features are similar, but just appear in different tissues. For example, when a patient has one autoimmune disease, they often develop or become susceptible to developing some features of other named autoimmune diseases,” Eggleton noted.
“As biomedical scientists that work to develop drugs to treat autoimmune diseases, we realise that many of the proinflammatory cytokines prevalent in most autoimmune diseases are the same, e.g., TNF, IL-6, IL-17 etc. We also know that most therapies for them focus on inhibiting pro-inflammatory pathways. But this approach itself will not cure a disease, but simply suppress the symptoms.” It was Eggleton’s opinion that it would be far better to attempt to ‘reset’ the pro- and anti-inflammatory balance by inducing immune homeostasis and re-educating the immune system to generate anti-inflammatory cytokines. For example, IL-10, for just as long is required before returning to basal levels.
- Bispecific T Cell Engagers and Synthetic Immunity: Circumventing Immune Escape
- ABclonal’s Novel Single B-Cell Based Platform for Monoclonal Antibody Discovery
There are very few single pathways that can be targeted to reset the immune system. The pharmaceutical and biotech industry is turning to cell therapeutics: CAR T cells, CAR T regulatory cells, and the manipulation of dendritic cells. They are doing so, Eggleton explained, “because many diseases have multiple pathways that become dysfunctional—it’s the same common defective pathways in different organs that become impaired, producing different forms of autoimmune disease.” By developing whole cell therapeutics in vitro or in vivo, one may be able to repurpose a cell treatment to work in multiple autoimmune and inflammatory diseases.
Early-Stage Lung Inflammation: Implications for Chronic Autoimmune and COVID Disease
Eggleton then recounted a study of patients with bronchiectasis, a rare and severe lung disease of the lung. Bronchiectasis presents when the airways become widened with a thick layer of mucus, which makes patients’ airways a breeding ground for bacteria— “you end up in hospital about four or five times a year.” As Eggleton noted, another complication that sometimes arises from bronchiectasis is rheumatoid arthritis: “So, we thought that there could be a link between lung disease and autoimmune disease – particularly RA.”
“We ran a study at Exeter University Medical School with bronchiectasis patient samples collected from centres in the North-East, South-West, and the Midlands of England. We found that many patients with chronic bronchiectasis had a breakdown of immune tolerance which was not citrulline-specific during the early stages of developing autoimmunity. Furthermore, we found that it became more specific in patients with bronchiectasis in whom rheumatoid arthritis develops. Smoking, which also damages the lungs, is a high-risk factor for going on to develop rheumatoid arthritis. This begs the question ‘is the lung an initiating site of tolerance breakdown prior to developing autoimmune disease many years in the future’?”
Eggleton said that a similar inflammatory process of lung pathology was happening during the pandemic. COVID-19 is another disease of the lung that causes extensive inflammation, much like bronchiectasis, and activates many of the same pro-inflammatory cytokines and cells. Consequently, drugs that were originally approved for use against autoimmune diseases like RA were repurposed for use against COVID-19. An unfortunate supply and demand feature of this was shortages in anti-inflammatory rheumatological medicines emerged during the hight of the COVID pandemic. This was due to the demand of some of these rheumatological drugs being reassigned for treating COVID patients. Eggleton said "it will be of interest to monitor patients with long COVID to see if they develop autoimmune disease with a greater frequency than the non-COVID population in the future.”
The panel discussion then concluded with a question-and-answer session between the audience and panellists.
At Tumour Microenvironment: In Person, learn about recent advances in tumour microenvironment research at the basic, translational, and clinical application levels, with exploration of the latest biomarker and spatial technologies to better understand the tumour microenvironment, alongside emerging therapeutic opportunities in immuno-oncology.








