Using Organs-on-Chips to Catch Kidney Toxicity in Drug Discovery
Edited by Tom Cohen
Anna-Karin Sjögren is a Director and Discovery Safety Specialist for AstraZeneca. At Preclinical Organ Modelling UK 2022, Sjögren provided a perceptive presentation on the work that AstraZeneca have been doing in using an organ-on-a-chip to evaluate drug-induced kidney toxicity during drug discovery.
Sjögren said that advanced in vitro models were required to assess toxicity because kidney-related drug attrition is still a concern during drug discovery and development. “Quite often,” Sjögren added, “this is because the toxicity is discovered pretty late.”
- Challenges in Developing Organoids for Neuroscience
- Experts Discuss Next Generation Organoids: Challenges and the Future
- Tackling Tumours In-Vitro with 3D Cell Cultures
Discussing the keys to success in developing useful in vitro kidney toxicity models, Sjögren explained that having enough physiological relevance in your models is vital. Furthermore, “it is also important to consider what toxicity endpoints to use,” Sjögren added. “It has been beneficial to include multiple endpoints that reflect more subtle changes. For example, the functional changes, rather than just cell death.”
Above all, Sjögren recommended that a fit-for-purpose approach should be taken for organ modelling: “what is the most appropriate model for the questions you have?” The more complex models, such as MPS come with lower throughput, lower turnaround, and higher cost, “so, it’s important to consider those factors when choosing your models.”
As Sjögren justified however, there are reasons why researchers would want to use the more complex models. For example, “you may want to look at a specific mechanism; perhaps you have a compound which has shown kidney toxicity in in vivo studies, and you want to look at backup compounds? Or you may want to distinguish between a few compounds before you decide on your lead compound.” In those and in other cases, Sjögren sees that a more complex model could be beneficial.
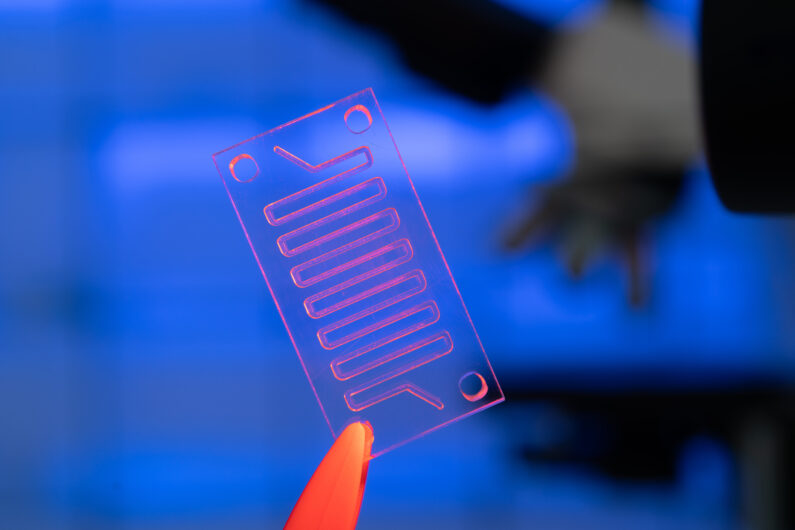
Kidney-On-a-Chip Models
Sjögren’s team at AstraZeneca have been studying kidney-on-chip models to incorporate flow, 3D structures, and extra-cellular matrices for improved physiological relevance to human kidneys. Since most kidney toxicity caused by drugs is seen in the proximal tubule, AstraZeneca have focused their attention on renal proximal tubule epithelial cells (RPTECs).
Sjögren pointed out that there are “of course, different applications for this kind of system.” She gave two examples which they can study in this regard: transport-dependent and polarisation-dependent toxicity, and long-term drug induced kidney toxicity.
Membrane-Dependent Cisplatin Toxicity in the Proximal Tubule-On-a-Chip
The AstraZeneca team set up their dual channel chips to study membrane dependent cisplatin toxicity in the proximal tubule for a proof-of-concept test. Cisplatin is known to be taken up by the OCT2 transporter located on the basolateral side of the proximal tubule.
To study this in vitro, Sjögren’s team exposed cisplatin in the empty channel and, when mimicking a basolateral exposure, saw that this induced toxicity. The toxicity that they observed was evidenced by changes in morphology and via a reduction in cell count.
Next, to validate the experiment, they exposed the cisplatin in the apical channel and saw no change in the morphology of the cells, nor did they see a reduction in cell count, or an impact on the membrane integrity. “This demonstrates how this could be a beneficial model if you think you are dealing with a mechanism that involves drug transporters,” concluded Sjögren.
Replicating ASO-Induced Nephrotoxicity
Another experiment that AstraZeneca were interested in studying was replicating kidney injury biomarker response induced by nephrotoxic antisense oligonucleotides using kidneys-on-chips. “Antisense oligonucleotides (ASO) are a therapeutic modality of increased interest,” Sjögren noted, adding that “while toxicity assessments for small molecules have really improved, other modalities are lagging behind.”
Sjögren noted that certain ASOs have caused nephrotoxicity in the clinic. For example, SPC5001 caused acute kidney injury in one clinical trial. In the study that Sjögren showcased, they used SPC5001 as a tool ASO to define the predictive value of a proximal tubule-on-chip model for kidney toxicity. This study looked at gene expression, cytotoxicity, and kidney injury biomarkers.
Cytotoxicity was induced by SPC5001 only and not by a control ASO used as negative control. In addition, SPC5001 increased perfusate levels of kidney injury biomarkers, including KIM-1 and NGAL, with distinct time-dependent profiles.
“The beauty of kidney-on-a-chip,” said Sjögren, “is that you can see over time, rather than just having a snapshot – this is useful due to the time dependency of some of these effects.”
Sjögren’s talk showcased proof of concept data for the utility of her team’s kidney-on-chip models. Furthermore, it stresses the importance of organ modelling being fit-for-purpose and not just “going complex for the sake of it.” Going forward, Sjögren says that she would like to see the field expanding into new modalities other than just small molecules and ASOs.
Want to discover what’s next in the industry? Discovery US: In-Person will address drug discovery in new modalities such as protein degradation, and case studies on the integration of screening approaches in phenotypic and genomics-based discovery, Organ-on-a-chip and 3D modelling.