Organoids: Opening New Doors for Cancer Research
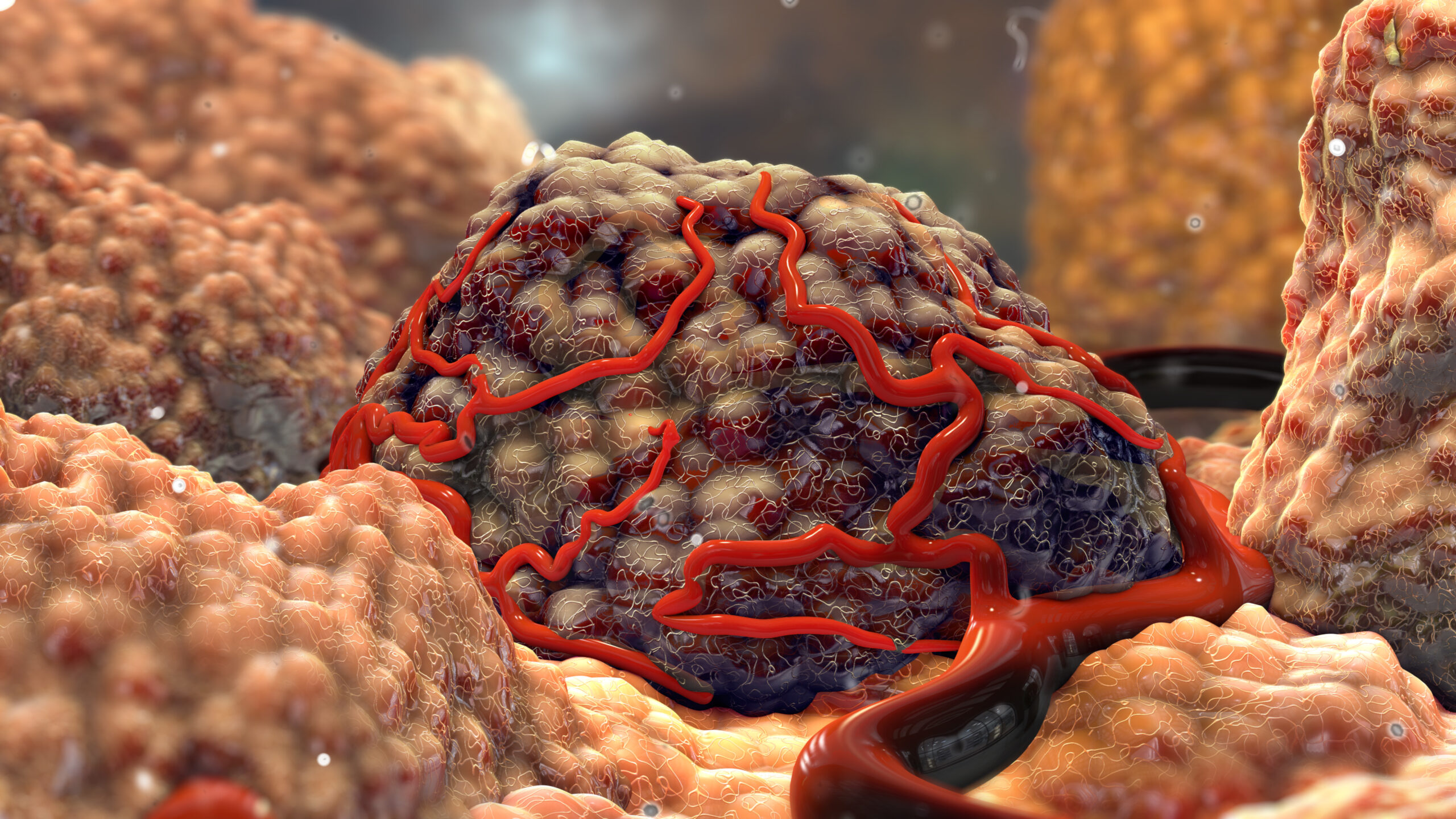
Organoids are three-dimensional tissue cultures grown from stem cells. They have been among the most important and exciting developments in medical sciences in the last decade. Their ability to replicate the biology of diseased and healthy organ tissue in vitro is helping us understand complicated disease mechanisms and replace faulty cells within the body.
Application and Uses
Organoids allow the creation of virtually limitless amounts of tissue. Testing of tissues is particularly valuable for rare diseases. Developing treatments for rare diseases is difficult due to small patient populations, an issue that could be dramatically mitigated with organoid use. For example, close to half of all cystic fibrosis patients have the disease due to a rare genetic defect, in many cases only affecting tiny populations and, in some cases, single family lines. The time and money to develop new treatments for each of these genetic defects is sadly not feasible. Fortunately, organoids derived from patients have been used to test if they would respond to existing drugs that would otherwise not be approved due to the expense and risk of administering them to non-receptive patients.
Besides use in rare disease research, organoids have incredible potential for oncology. Tumour organoids open several new doors for cancer research. Compared to other methods, they are better suited to scaling, with the additional advantage of being more translatable to in vivo models due to their unique similarities to actual tumours. These applications range from investigating basic disease biology and drug response screens to potentially revolutionising the traditional drug development workflow. Using tumour organoids could shift this workflow from a linear to high throughput matrix process, allowing for simultaneous selection of target patient populations and lead candidates.
Patient Derived Organoids
Leo Price, from CrownBio, explains that both healthy tissue and tumour patient-derived organoids can be grown “from the same patient, so basically, we can derive organoids from the healthy tissue, for example from healthy epithelium adjacent to the tumour, and then also have tumour organoids which allows us to run comparative experiments side by side. I think that has a massive benefit compared to other forms of 3D culture, whether it’s spheroids or cell lines, where obviously the healthy tissue is not available”. Several studies have shown that organoid biology more closely reflects patient tumour biology than conventional cell culture. Another advance in in vitro to in vivo translation is achieved by using the tumour organoids to generate Patient Derived Xenografts (PDX). Here the in vitro and in vivo tumours are genetically identical.
Testing a new therapeutic in just one tumour model is never sufficient and a typical in vitro strategy is to test in a panel of tumour cell lines. A downside to this approach is that those cell lines are typically generated and propagated through diverse methodologies and with different media. Organoid technology is well standardised and large panels of organoids have been generated using identical proceedures. This improves the ability to attribute differential drug responses to specific mutations or sub-classes.

What’s next for tumour organoids?
There are still some challenges ahead for the widespread use of tumour organoids. Last April, at our Organoid Discovery Symposium, we held a panel discussion titled ‘Advancing Organoids in Oncology Drug Development’. One area that came up repeatedly was the timescale required to grow functional organoids.
Organoids grow much more slowly than traditional cultures, where cancer line lines have been observed doubling in as little as twenty-four hours. This can have a massive impact, particularly in the case of oncology.
Gaston Soria shares his experience, stating that he has “discussed growth rates with several oncologists around the world; they said that would need to get a response within two or three weeks for viability in the clinic.
He continued to explain the challenges with implementing organoid technology “we know that the time frame is quite short for an organoid setup into ex vivo drug testing. If we want to want to move the organoid technology into the ex vivo testing of drugs in the clinic, we may need also to explore some hybrid technology. The downside is that may lessen the fidelity of the model but in return give us a bit of speed that we need for cancer patients.”
Leo Price offers an alternative viewpoint, arguing that “These organoids grow slowly, but that is actually a good model of what we see in patients – tumours do not double in cell number every 24 hours like many cell lines. While that makes it a little harder to keep the aggressive timelines that we all are living with, it pays off in the quality of the biology that is allowed to develop.”
Final Thoughts
Organoids have received increasing attention over the past decade and is already showing real-world results. There are high hopes that they will transform our understanding of cancer, unlocking new treatment options and alternative therapies with far fewer side effects than our current methods.




.png)